Contusion - contusio cerebri
A brain contusion is severe traumatic brain injury in which the brain is damaged, unlike a concussion with no or minimal brain damage.
Like bruises in other tissues, cerebral contusion can be associated with multiple microhemorrhages, small blood vessel leaks into brain tissue. Contusion occurs in 20–30% of severe head injuries.
With a brain contusion, there is always loss of consciousness for at least fifteen minutes, and the loss of consciousness is deeper than in case of a concussion.
By the force of the blow or impact to the head, a bruising of the brain tissue is created.
Brain tissue is broken and the brain is oppressed by blood and fluid (swelling).
This means there is extensive and complex damage to the brain. Since cerebral swelling presents a danger to the patient, treatment of cerebral contusion aims to prevent swelling.
Due to the danger of increased intracranial pressure, surgery may be necessary to reduce it. People with cerebral contusion may require intensive care and close monitoring.
Depending on the severity and location of the bruising, effects differ.
One person with cerebral contusion may recover almost completely and the other can keep on suffering from severe disabilities.
The long-term effects of moderate to severe TBI can include challenges with attention span and the ability to concentrate and remember. These are known as cognitive problems. Difficulties with processing input from the senses, such as touch, vision, hearing, taste and smell may also occur. Other effects can include, seizures, chronic pain, sleep disorders, loss of bladder or bowel control, and a variety of social and emotional challenges.
A severe traumatic brain injury involves an unconscious state or coma that lasts days, weeks, months, or even years. Typically, the greater the amount of brain damage, the longer a person remains in a coma, and the more challenging the recovery may be.
| It’s important to keep in mind that every traumatic brain injury is different, and every person responds differently. |
| The symptoms and effects will vary greatly from one patient to another, depending on i.a. the severity of the TBI. |
SEQUELA
Possible sequelae are divided into categories:
- physical problems
- emotional and personality changes
- motoric disorders
- psycho-social problems
- cognition (see list below for cognitive impairment)
After a TBI, neurons (nerve cells) in the brain may be damaged. As a result, the neurons may have trouble doing their job of carrying signals to different parts of the brain. As a result, if you have a brain injury, you could have trouble thinking or moving as you normally do. Your brain may also have trouble keeping your body working properly.
The great need for structure in daily life is striking!
A typical phenomenon associated with brain injury, is the disharmonious profile: for example, a high IQ on the verbal level, but markedly lower at the executive level (such as organizing or perpetrating of acts). The pace of thinking can also be affected.
COGNITIVE DISORDERS
Cognitive disorders are related to cognition: thinking, language, memory, concentration, processing knowledge, perception, awareness, and attention. So it is a broad term.
In patients with brain contusion these disorders can express themselves in the following ways:
- impaired intellectual functioning (sometimes only partial)
- delays in the processing of information (mental slowness)
- attention deficits
- memory problems
- orientation Issues
- visual-spatial problems
- problems with coordinating daily and / or complex actions (apraxia)
- problems in identifying things or issues
- language problems
- problems with calculation
- problems with executive functions
COUP AND CONTRA COUP
The brain is the most complex and vulnerable part of the human body. It has a composition resembling a gelatin like structure.
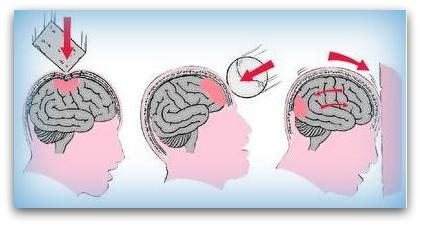
A common way that a person can experience a traumatic brain injury is when an impact or violent motion brings their head to a sudden stop causing the brain to slam into the skull.

This is called a coup contrecoup injury also known as an acceleration deceleration injury In this kind of injury the brain bounces back and forth inside of the head causing damage to the brain where it hits the skull The brain is injured at the point of direct impact and because it bounces back into the opposite side of the skull the opposite side of the brain is injured as well.
Coup contrecoup injuries can involve damage to the brain at the specific point of impact called focal injuries or to a large part of the brain known as diffuse injuries It s important to know that coup contrecoup injuries can happen as the result of trauma without direct impact to the head since it is the movement of the brain inside of the skull that causes the injury.
You see in the video below on the side of the blow swelling, bruising and tearing of blood vessels. This is called a 'coup'.
Because the brain moves slower than the skull, the brain first clashes against the bone on the side of the blow.
But then the brain will go against the back of the skull to collide. This is called a "counter-coup."
Also at the back occurs bruising and tearing of blood vessels. Both front and back are now damaged. See videos below:
On a microscopic level, not visible on an MRI scan, the braincel body can tear off from the axons. The axons give signals to the different brain bodies.
After the tear both axons and the brain-body die within seconds. These dead brain cells cannot communicate with each other ...!
In the dying process chemicals are released; neurotransmitters. They provide even more damage. The lesion then spreads in the immediate vicinity of the affected brain cells. That damage can last up to 24 hours after the initial impact. That is why the first 24 hours after the accident are so crucial.
LIST OF COMPLAINTS AFTER brain contusion
The brain contusion CCF Foundation has published the list below.
"Top 14 of complaints as reported by contusiopatients, 12 months after the accident, with decrease of Trauma Complaints List (Of Zomeren and Van den Burg, 1985). Frequencies are percentages of affirmative answers. Notice that headache, contrary to what you might expect, is not the most frequently given answer."
49% forgetfulness
41% increased fatigability
39% increased need for sleep
36% irritability
34% of inertia
31% concentration
30% sensitivity for crowds
27.5% dizziness
26% sensitivity to noise
25.5% loss of initiative
25.5% headache
21% easily overwhelmed by emotions
21% inability to do two things at once
19% depressed mood
POST TRAUMATIC STRESS DISORDER/ PTSD
Posttraumatic stress disorder (PTSD) is a severe stress reaction to a shocking event. It is also a natural reaction to an unnatural event.
There is a chance that someone with the rise of traumatic brain injury also develops PTSD, as the cause of the brain injury was a very shocking event. For example in:
- natural disasters
- aircraft accidents or serious car accidents
- terrorist attacks
- assault with violence causing brain injury
- rape by force, causing brain damage
- robbery with violence, causing brain damage
- confrontation with someone who is seriously injured or slain and spearheading this experience
- war experiences
Post-traumatic stress disorder has the following characteristics:
Extreme loss of control. People are losing their grip on daily life. Many victims feel powerless.
Disruption: Obvious expectations no longer apply. Confidence in themselves, other people and everyday life is gone. One is faced with his own vulnerability.
Such a shocking event may cause a disruption of the psychobiological balance. People remain set at danger. The fear is permanent. This condition disrupts their daily lives, with the possible consequences:
- chronic stress
- excessive vigilance
- physical complaints
- reliving of the trauma
- nightmares / night Terrors
- fears
This situation needs to be treated by experienced neuro-psychologists who have knowledge of both brain and PTSD.
It may also be necessary to refer to (neuro)psychiatrists.