White Matter Abnorminalities WMA
Introduction
People often ask us what it means when white spots have been seen on a brain scan. It worries people. With this page we try to show that there can be many causes of white spots on a brain scan, but that there can also be innocent white spots on a scan.
Normally a brain scan shows the brain in gray-black. If white spots are visible and the patient has complaints, the doctor will want to rule out a disease.
The purpose of this page is to provide an explanation where medical terms sometimes remain incomprehensible and to link to the right information.
Ultimately, the doctor is the person who can provide the correct information about your situation.
If you want to quickly access information, choose whether multiple spots (multifocal) have been found, whether spots flow together (confluent) or whether a single separate spot (focal) has been seen.
See image below for clarification. The entire page contains a lot of information. We look at the possible causes per brain area and per pattern of spots.
In the image below we show what the different abnormalities can look like on a scan. The black areas in the middle of the image are cavities in the brain, also called ventricles.
- spots that merge = confluent
- a single loose spot = focal
- multiple spots (multifocal)

White matter and gray matter?
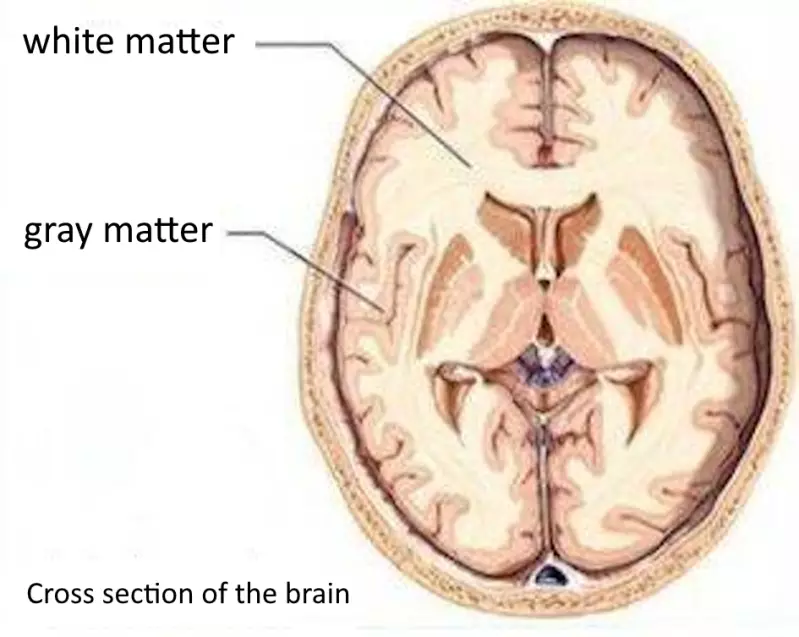
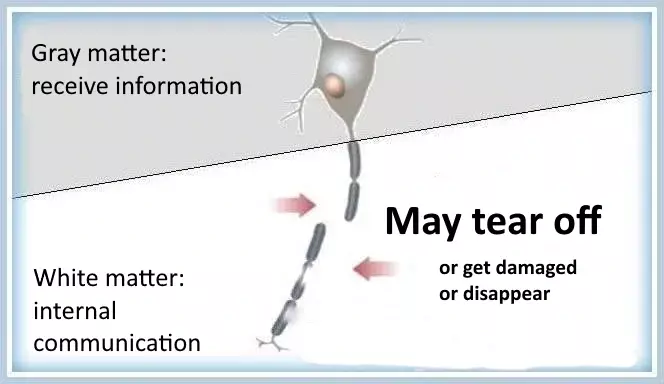
The brain consists of gray matter and white matter.
The white matter is located inside the brain. The gray matter is located on the outside of the brain.
The gray matter consists of the cell bodies of brain cells. Hence the expression 'your gray cells', which refers to the brain. The gray matter processes information.

Difference between white matter diseases and white matter abnormalities
First of all, not every white matter abnormality is a disease.
White spots on a brain scan also occur in healthy elderly people.
Not every white matter abnormality is a white matter disease.
Sometimes a white matter disease is discovered because white matter abnormalities are visible on a scan.
White matter disease
A disease of the white matter, in which the protective layer of the long processes / myelin is damaged and is slowly broken down,
is called white matter disease (leukodystrophy).
These diseases progress in severity (progressive) with breakdown of the myelin (degenerative). An example of this is MS/multiple sclerosis.
White matter diseases are usually hereditary conditions that manifest themselves in babies and young children.
The apparently healthy children slowly become sicker.
They lose muscle mass and deteriorate in movement, walking, seeing, hearing, speech and behavior.
Sometimes there is no hereditary condition, but the disease develops spontaneously. That's called a mutation. In some cases the disease only manifests itself in adulthood.
There are about a hundred different diseases of the white matter (white matter diseases). We won't cover all of them here. Follow this link for more info.
White matter abnormality
A white matter abnormality (WSA) is the term for a finding on a brain scan. A 'radiological finding of white spots'. That can mean anything and we try to explain that on this page.
White matter abnormalities often cause problems such as slow thinking, memory problems, difficulty with executive functions (cognitive disorders), problems with walking or depression.
Causes of white matter abnormalities
White matter abnormalities (WMA) can have many causes. This also makes it difficult to determine what is going on. As we wrote earlier, having a white matter abnormality does not in itself indicate whether someone is ill.
The doctor will still want to rule out a few things: an inflammatory disease (possibly with reduced myelin), infectious disease, blood vessel disease, brain injury due to an accident, brain tumor or metastasis, metabolic disease, poisoning, etc.
The doctor will want to know
- whether there has been chemotherapy or radiation
- whether there are eye complaints
- whether there is a thyroid condition
- whether there is depression
- whether there is cognitive decline (for example
difficulty with memory and/or concentration) - whether a lot of alcohol or drugs has been used
- whether someone has cardiac arrhythmias
- whether someone has epileptic seizures
- whether someone has high blood pressure
- whether anyone is familiar with migraines
- whether there is loss of muscle strength
- etc.
A white matter abnormality is usually caused by a lack of oxygen in the cerebral blood vessels.
High blood pressure and arteriosclerosis can be the risk factors. A study showed that there is a connection
between arteriosclerosis of large blood vessels and dementia.
Problems with memory or concentration can be a precursor to developing dementia. Cognitive dysfunction is directly related to white matter abnormality and can ultimately lead to vascular dementia, especially the rare Binswanger disease/subcortical leukencephalopathy.
At Alzheimer's disease, there appears to be a connection between the severity of white matter abnormalities on an MRI scan of the brain and low concentrations of vitamin B 6 in the blood. More research on this is needed prove this.
Sometimes a very small infarction (lacunar infarction) or a very small cerebral hemorrhage (microbleed) occurs. Sometimes the spaces surrounding blood vessels of the brain (the Virchow Robin spaces
or perivascular space/PVS) slightly enlarged. This is also seen as white spots on the scan. That is not necessarily an unusual situation. This happens to about half of the people.
A cause is not always found for the deviations. Sometimes there is a genetic cause that is inherited.
Indications for a diagnosis
Listening to complaints and physical examination Before a doctor decides on a brain scan, the patient's story about the complaints is carefully listened to and the doctor conducts a physical examination.
Pattern on the scan Sometimes a typical pattern can be distinguished in the spots on a brain scan. This can be an important indication for the doctor in which direction to look for a diagnosis.
Brain area on the scan It is important to recognize in which area of the brain the spots are visible. That is also an important clue towards diagnosis.
Age The age at which the white matter abnormality is found can also help make a diagnosis. Aging people more often have white matter abnormalities with innocent causes or indicative of a form of dementia or Alzheimer's.
Visible patterns on a brain scan
The brain scan is checked to see if
- a single loose spot is visible (focal)
- there are multiple spots (multifocal)
- the spots merge and merge into the gray matter (confluent)
Sometimes a single spot is visible at the beginning of a disease and later the spots may have merged somewhat. Therefore, based on the complaints, the doctor will also decide whether or not to have another brain scan done.
Focal (local) white matter abnormalities
If a single spot is seen, the question is whether the spot is near the
brain beam (corpus callosum), in the middle of the cerebral hemispheres. Subsequently, the use of contrast fluid (gadolineum enhancement) by infusion during the brain scan is recommended, because this makes it possible to distinguish between possible diagnoses.
- Near the brainbar (corpus callosum)
- with contrast fluid
- a brain tumor: lymphoma (growth of the lymphatic system)
- an inflammatory disease such as Multiple Sclerosis / MS or systemic lupus erythematosus/SLE, an autoimmune disease in which something goes wrong with the immune system
- a poisoning/toxic cause: Marchiafava Bignami disease, which is associated with heavy alcohol consumption
- without contrast fluid
- a brain tumor (low-grade glioma)
- traumatic brain injury such as brain contusion (contusio cerebri) or diffuse axonal damage/DAI
- with contrast fluid
- Not near the brainbar (corpus callosum)
- with contrast fluid
- brain tumor: lymphoma / tumor of the lymphatic system or metastasis
- traumatic brain injury, cerebral contusion (contusio cerebri) or diffuse axonal damage /DAI
- infectious disease: brain abscess, CMV/cytomegalus virus/herpes virus or human herpes virus 6/HHV-6
- without contrast fluid
- brain tumor (low-grade glioma)
- traumatic brain injury contusio cerebri or diffuse axonal damage/DAI
- blood vessel related/vascular: oxygen deficiency (ischemia)/ cardiac arrhythmia/atrial fibrillation/atrial fibrillation, cerebral infarction or migraine
- infectious disease, malaria or Creutzfeldt-Jakob disease /CJD
- with contrast fluid
Multifocal white matter abnormalities (in multiple locations)
In case there are multiple spots, doctors mainly investigate in which brain area the spots are located.
- Cortical (in the cerebral cortex)
- blood vessel related/vascular: blood vessel inflammation/vasculitis
- metabolic disease/metabolic: MELAS /mitochondrial encephalomyopathy, a disease of the energy factories of the cells
- infectious disease/infectious: Creutzfeldt-Jakob disease /C.J.D
- inflammatory disease / inflammatory: Progressive multifocal leukoencephalopathy/PML or Acute Demyelinating EncephaloMyelitis / ADEM
- Subcortical (under the cerebral cortex)
- blood vessel related/vascular: oxygen deficiency; possible cerebral infarction or cardiac arrhythmia/atrial fibrillation/atrial fibrillation (ischemic WSA), blood vessel inflammation/vasculitis,
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy / CADASIL, Cerebral Amyloid Angiopathy / CAA, migraine, primary angioitis of the central nervous system / PACNS and depression in elderly people - metabolic disease/metabolic: Fabry disease/alpha-Galactosidase, chronic progressive external ophthalmoplegia/CPEO with complaints of the eye muscles
- infectious disease / infectious: Lyme disease / Borrelia burgdorferi, lues, Herpes simplex virus / HSV, human herpesvirus6 / HHV-6 or Progressive multifocal leukoencephalopathy/PML
- inflammatory disease/inflammatory: Multiple sclerosis /MS, Balo's disease, Sjögren's syndrome, sarcoidosis, NMO/Neuromyelitis Optica or inflammatory bowel disease
- poisoning/toxic: chemotherapy, carbon monoxide poisoning/CO intoxication, immune system suppressing drugs/immunosuppressants.
- brain trauma: diffuse axonal damage /DAI or
brain contusion / contusion of the brain
- blood vessel related/vascular: oxygen deficiency; possible cerebral infarction or cardiac arrhythmia/atrial fibrillation/atrial fibrillation (ischemic WSA), blood vessel inflammation/vasculitis,
- Periventricular (around the cerebral cavities/side ventricles)
- blood vessel related/vascular:oxygen deficiency; possible
cerebral infarction or cardiac arrhythmia/atrial fibrillation/atrial fibrillation ischemic WSA, Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy/CADASIL,Cerebral Amyloid Angiopathy/CAA, Cognitive function disorders - metabolic disease/metabolic: vitamin B12 deficiency/deficiency
- MELAS/mitochondrial encephalomyopathy;
a disease of the energy factories of the cells, the mitochondria - infectious disease/infectious: Creutzfeldt-Jakob disease /CJD,
CMV/cytomegalus virus (herpes virus) or human herpes virus
6 / HHV-6, brain inflammation due to the herpes simplex virus /HSV - encephalitis inflammatory disease/inflammatory:
Acute Demyelinating EncephaloMyelitis / ADEM, Multiple sclerosis/MS - poisoning/toxic: chemotherapy, Wernicke encephalopathy,
- miscellaneous: radiation/radiotherapy or hydrocephalus
- blood vessel related/vascular:oxygen deficiency; possible
- At the basal nuclei (basal ganglia)
- blood vessel related/vascular:
oxygen deficiency possible due to cardiac arrhythmia/atrial fibrillation/atrial fibrillation, cerebral infarction
/ischemic WSA, blood vessel inflammation/vasculitis,
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy / CADASIL - metabolic disease/metabolic: Fabry disease/alpha-Galactosidase
- infectious disease/infectious: Creutzfeldt-Jakob disease/CJD
- inflammatory disease/inflammatory:
Acute Demyelinating EncephaloMyelitis / ADEM - poisoning/toxic: carbon monoxide poisoning / CO intoxication or copper stacking/Cu stacking
- blood vessel related/vascular:
- At the brainbar (corpus callosum)
- blood vessel related/vascular: Susac's syndrome
- metabolic disease/metabolic: leberoptic neuropathy with single-sided visual impairment, extrapontine myelinolysis, Wernicke encephalopathy
- infectious disease/infectious: human immunodeficiency virus/HIV, malaria in the brain/cerebral malaria
- inflammatory disease/inflammatory: Acute Demyelinating EncephaloMyelitis / ADEM, Multiple sclerosis /MS or Progressive multifocal leukoencephalopathy/PML
- poisoning/toxic: Marchiafava Bignami disease, which is associated with heavy alcohol use
- traumatic brain injury/trauma: diffuse axonal damage /DAI or brain contusion / contusion of the brain
-
Infratentorial (under the tentorium cerebelli; this concerns the cerebellum and the brainstem)
- blood vessel related/vascular: migraine
-
metabolic disease/metabolic: pontine myelinolysis, X-ALD, a metabolic disease fully called X-linked adrenoleucodystrophy or Siemerling-Creuzfeld. The X indicates that the disease is caused by an error on the X chromosome
-
inflammatory disease/inflammatory: Multiple sclerosis /MS,
Acute Demyelinating EncephaloMyelitis/ADEM, NMO/Neuromyelitis Optica -
brain tumors/neoplasms:
low-grade glioma or brain metastases
Confluent
A diffuse, confluent white matter abnormality is also called
called leukoaraiosis.
In the case of confluent white matter abnormalities, it is examined whether it is spread throughout the brain (diffuse).

- Is it in the posterior cranial fossa?
The question of whether or not it is visible in the posterior cranial fossa excludes or confirms diseases. The posterior cranial fossa is the part on which the cerebellum rests. It is the part of the skull located furthest back in the brain (see this picture).- In case it is located in the posterior cranial fossa, there are a few possible diagnoses:
- oxygen deficiency in the blood vessels (vascular)
- inflammatory diseases such as: progressive multifocal leukoencephalopathy/PML, human immunodeficiency virus/HIV, encephalitis due to herpes simplex/HSV encephalitis
- a gliomatosis (a brain tumor)
- radiation poisoning
- a metabolic disease such as Hashimoto encephalopathy /SREAT. The full name of the latter condition is 'steroid-responsive encephalopathy' associated with autoimmune thyroiditis', where inflammation of the thyroid gland can in some cases cause the brain disease. Often this is accompanied by epileptic seizures.
- In case it is not visible in the posterior cranial fossa, the brain may be diseased due to:
- high blood pressure (hypertensive encephalopathy) (vascular)
- poisoning/toxication due to immune system suppressing medications
- by chemotherapy.
- In case it is located in the posterior cranial fossa, there are a few possible diagnoses:
- Is it not diffuse but at the level of the frontal lobe / frontal)? If this is the case, two serious metabolic diseases remain:
- Is it not diffuse but at the level of the parietal lobe or occipital lobe? If so, three causes with multiple syndromes remain:
- blood vessel related / vascular: diseased brain due to high blood pressure / hypertensive encephalopathy
- a leukodystrophy (for example Krabbe's disease or it indicates X-ALD; a metabolic disease that is also called adrenoleucodystrophy or Siemerling-Creuzfeld. The X indicates that the disease is caused by an error on the X chromosome
- a poisoning (toxic situation) due to heroin use, or due to immune system suppressing medication, or due to the Posterior Reversible Encephalopathy Syndrome / PRES
- Is it not diffuse but at the level of the cerebral cavities, also called ventricles or cerebral chambers? Then it can indicate three causes.
- blood vessel related/vascular in an advanced stage
- a metabolic disease such as Krabbe disease and Metachromatic leukodystrophy / MLD
- an inflammatory disease such as advanced multiple sclerosis
- Hashimoto encephalopathy /SREAT. The full name of the latter condition is 'steroid-responsive encephalopathy associated with autoimmune thyroiditis' where inflammation of the thyroid gland can in some cases cause the brain disease. This is often accompanied by epileptic attacks or Acute Demyelinating EncephaloMyelitis / ADEM.
- blood vessel related/vascular in an advanced stage
Many possibilities. Need more research?
Anyone who reads carefully will see that there can be overlaps in diagnoses when looking at the classification of the spots per brain area.
That is why the doctor will perform several examinations depending on the complaints.
It is wise not to do your own research via this page. The doctor is trained for this and it is the doctor's job to provide a good explanation.
The purpose of this page was to provide an explanation where medical terms sometimes remain incomprehensible and to link to the right information.
Resources
Briley D.P., Wasay M., Sergent S.., et al. Cerebral white matter changes (leukoaraiosis), stroke, and gait disturbance J Am Geriatr Soc 1997; 45: 1434-1438
Hersenletsel-uitleg
Hofman A, Ott A, Breteler MMB, Bots ML, Slooter AJC,Harskamp F van, et al. Atherosclerosis, apolipoprotein E, and prevalence ofdementia and Alzheimer's disease in the Rotterdam Study.
Lancet1997;349:151-4.
Liao D, Cooper L, Cai J, Toole JF, Bryan N, Burke G, etal. The prevalence and severity of white matter lesions, their relationshipwith age, ethnicity, gender, and cardiovascular disease risk factors: theARIC
Study. Neuroepidemiology 1997;16:149-62.
Leeuw FE de, Groot JC de, Achten E, Oudkerk M, Ramos LMP,Heijboer R, et al. Prevalence of cerebral white matter lesions in elderlypeople: a population based magnetic resonance imaging study. The
RotterdamScan Study. J Neurol Neurosurg Psychiatry 2001;70:9-14.
Leeuw FE de, Groot JC de, Gijn J van, Wittestofafwijkingen in de hersenen bij ouderen:vsculaire risicofactoren en mentale gevolgen. Ned Tijdschr Geneeskd. 2001;145:2067-71
Miedema.I.
https://www.nervus-online.nl/artikelen/kopie-van-artikel/t/wittestofafwijkingen-vanuit-een-klinisch-perspectief
Mulder C, Scheltens P, Barkhof F, Gundy C, Verstraeten RA, Leeuw FE de. Low vitamin B6 levels are associated with white matter lesions in Alzheimer’s disease. J Am Geriatr Soc. 2005;53:1073-4.
van Norden,A.G.W., Meijer, F.J.A., van Dijk, E.J., de Leeuw, F-E. Differential diagnosis of white matter abnormalities in adults: a systematic approach based on MRI. ‘The ABC’s of white matter abormalities’
https://www.ariez.nl/wp-content/uploads/2018/08/148-67.pdf I.W.M. van Uden,
Schmand B, Jonker C, Hooijer C, Lindeboom J. Subjectivememory complaints may announce dementia. Neurology 1996;46:121-5.
Olszweski J., Subcortical arteriosclerotic encephalopathy. Review of the literature on the so-called Binswanger's disease and presentation of two cases World Neurol. 1962; 3: 359-375
O'Sullivan M., Leukoaraiosis Pract Neurol. 2008; 8: 26-38
de Leeuw FE, de Groot JC, Achten F, et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study-the Rotterdam Scan Study J Neurol Neurosurg
Psychiatry 2001; 70: 9-14
Tolman, C.J. |Lycklama à Nijeholt, G.J. op 14-03-2017
https://www.nervus-online.nl/tijdschrift/editie/artikel/t/wittestofafwijkingen-bij-volwassenen
Tomimoto H., Akiguchi I., Akiyama H., et al. Vascular changes in white matter lesions of Alzheimer's disease Acta Neuropathol (Berl) 1999; 97: 629-634
Wiszniewska M., Devuyst G., Bogousslavsky J. et al., What is the significance of leukoaraiosis in patients with acute ischemic stroke? Arch Neurol., 2000; 57: 967-973
Whitman G.T. Tang Y., Lin A., et al. A prospective study of cererbral white matter abnormalities in older people with gait dysfunction Neurology 2001; 57: 990-994
Wolf H, Ecke GM, Bettin S, Dietrich J, Gertz HJ. Do whitematter changes contribute to the subsequent development of dementia inpatients with mild cognitive impairment? A longitudinal study. Int J
GeriatrPsychiatry 2000;15:803-12.
https://nl.wikipedia.org/wiki/Leukoaraiose
MRI scan door Yakafaucon - Eigen werk, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=4412679