Heart patient or brain injury patient?
Heart diseases may cause brain injury
Research shows that the heart and brain are strongly connected and influence each other. They have the same risk factors.
Heart problems can have a major impact on the body and can even disrupt blood flow to the brain.
This can lead to a lack of oxygen or a stroke in the brain, which can result in cognitive problems or brain damage.
The word "cognition" refers to everything related to thinking. It refers to how your brain works
to perceive, understand, remember, and use that knowledge.
Symptoms of a lack of oxygen vary, from mild memory loss and difficulty concentrating to more serious neurological and neuropsychological problems. It is important to understand this connection. This allows doctors to make the correct diagnosis more quickly and begin the appropriate treatment and rehabilitation immediately.
Three common heart conditions in adult: heart failure, atrial fibrillation, and coronary heart diseas, are often associated with cognitive impairment. More information about these possible cognitive functions can be found behind the link.
List of heart diseases that may cause brain injury
- Atrial fibrillation is an irregular heartbeat that increases the risk of blood clots.
These clots may enter the bloodstream and become lodged in the brain's blood vessels, leading to
a stroke. - Valve disease may disrupt blood circulation, preventing the brain from receiving enough oxygen. This may lead to brain damage due to a lack of oxygen.
- A heart attack may severely disrupt the supply of blood and oxygen to the brain. This may lead to brain damage due to a lack of oxygen.
- Heart failure reduces blood flow to the brain, which may lead to brain damage due to a lack of oxygen.
Brain injury caused by heart failure is associated with changes in the parts of the brain important for thinking and emotions. It may result in cognitive impairment, mood problems, and a decrease in gray matter (brain cells) in various brain areas. In addition, it can accelerate brain aging and contribute to functional decline. - Cardiac arrest: If resuscitation is successful and the person survives, there is a chance that brain damage has occurred due to a period of oxygen deprivation.
Brain damage from cardiovascular disease may also, sooner or later, lead to vascular dementia.
It's important to seek immediate medical attention for symptoms such as confusion, decreased consciousness, dizziness, weakness, or speech problems to prevent permanent damage as much as possible. Read about all the symptoms of a stroke.
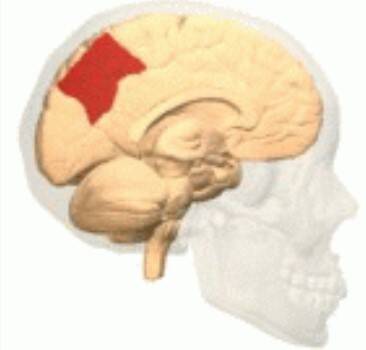
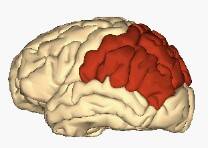
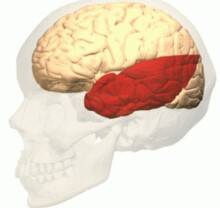
Brain areas primarily affected by heart failure or poor blood flow to the heart (ischemic heart disease)
Ischemic heart disease causes a decrease in gray matter (brain cells). This primarily affects the left frontal, right frontal, and lateral areas of the brain. It includes parts of the frontal lobe, the temporal lobe, and the parietal lobe (including the precuneus, a part of the parietal lobe).
Education about brain damage caused by heart problems is important
Educating heart patients about the potential effects of heart disease on the brain is crucial, during their hospital stay, after discharge or during an outpatient clinic visit.
It provides the patient, her or his partner and the family with the necessary insights and support.
If a heart patient refuses to believe that their heart problems have caused brain damage, this could indicate that they don't fully understand the potential consequences of cardiovascular disease. It could also be due to a specific consequence of brain damage: anosognosia, or lack of insight into the disease.
However, even more often, the subtle cognitive symptoms are barely noticeable, meaning those around them are often the first to notice the person's changes. It's also possible that the person increasingly notices that something is no longer going well, or that something is no longer happening as naturally. We call these invisible consequences of brain damage. After all, if the consequences had been physical, they would have been noticed much sooner.
A neuropsychological investiogation can identify the potential impact of a brain injury on functioning. Read more about this on our neuropsychological examination page.
We have developed a checklist for acquired brain injury to help people more quickly recognize which symptoms may be caused by brain damage. It's best if both the patient and their loved ones complete this checklist and compare their answers.
Do this at a calm moment and don't blame the other person for not recognizing something. Insights often come over time, when someone notices a few times that something is no longer working as well as it used to.
The page about determining whether you have a brain injury may also provide insight.
Conversely, acute brain injury may also cause heart problems
An acute brain injury, particularly a stroke, can cause a cardiac complication such as neurogenic stress cardiomyopathy (NSC).
The way the brain and heart interact is complex. It involves sympathetic nervous system activity, hormone release from the brain and adrenal glands, and the influence of the immune system and inflammation (hormonal processes of the hypothalamic-pituitary-adrenal axis).
Causes
Heart problems in neurogenic stress cardiomyopathy (NSC) can be caused by various neurological conditions, including traumatic brain injury, cerebral hemorrhage or stroke, central nervous system infections, and epilepsy.
Physical and emotional stress, grief, or anxiety can also trigger this condition, but not in everyone.
In approximately one-third of the patients, no clear cause of the symptoms can be found.
Symptoms
Symptoms of neurogenic stress cardiomyopathy are similar to those of a heart attack, such as chest pain, shortness of breath, and fainting, but there is no blockage of the coronary arteries.
It is therefore classified as a heart attack without a blockage in the coronary arteries.
Nevertheless, a doctor will initiate treatment.
Keywords: Cerebral hypoperfusion, cerebral blood flow disorder; cognitive impairment; brain injury, acquired brain injury, ischemia, cerebral hemorrhage, cerebral infarction, depression, neuropsychological disorders, heart failure, heart attack, cardiac arrest, cardiopulmonary resuscitation, valvular heart disease, coronary artery disease, ischemic heart disease, neurogenic stress cardiomyopathy (NSC)
Resources
- https://www.hersenletsel-uitleg.nl/soorten-hersenletsel-hersenaandoeningen/zuurstoftekort/hartpatient-of-nah
- Zhao B, Li T, Fan Z, Yang Y, Shu J, Yang X, Wang X, Luo T, Tang J, Xiong D, et al. Heart-brain connections: phenotypic and genetic insights from magnetic resonance images. Science. 2023;380:abn6598. doi: 10.1126/science.abn6598
-
Gorelick PB, Furie KL, Iadecola C, Smith EE, Waddy SP, Lloyd-Jones DM, Bae HJ, Bauman MA, Dichgans M, Duncan PW, et al; American Heart Association/American Stroke Association. Defining optimal brain health in adults: a presidential advisory from the American Heart Association/American Stroke Association. Stroke. 2017;48:e284–e303. doi: 10.1161/STR.0000000000000148
-
Almeida OP, Garrido GJ, Etherton-Beer C, Lautenschlager NT, Arnolda L, Alfonso H, Flicker L. Brain and mood changes over 2 years in healthy controls and adults with heart failure and ischaemic heart disease. Eur J Heart Fail. 2013 Aug;15(8):850-8. doi: 10.1093/eurjhf/hft029. Epub 2013 Mar 4. PMID: 23463084.
-
Lazar RM, Howard VJ, Kernan WN, Aparicio HJ, Levine DA, Viera AJ, Jordan LC, Nyenhuis DL, Possin KL, Sorond FA, et al; American Heart Association Stroke Council. A primary care agenda for brain health: a scientific statement from the American Heart Association. Stroke. 2021;52:e295–e308. doi: 10.1161/STR.0000000000000367
-
Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker-Smith CM, Beaton AZ, Boehme AK, Buxton AE, et al; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2023 update: a report from the American Heart Association. Circulation. 2023;147:e93–e621. doi: 10.1161/CIR.0000000000001123
-
https://www.ahajournals.org/doi/full/10.1161/STR.0000000000000476
-
Motamed M, Nunes JT, Udell JA. Stress cardiomyopathy. CMAJ. 2024 Sep 22;196(31):E1083. doi: 10.1503/cmaj.240269. PMID: 39313267; PMCID: PMC11426345.
-
Mrozek S, Gobin J, Constantin JM, Fourcade O, Geeraerts T. Crosstalk between brain, lung and heart in critical care. Anaesth Crit Care Pain Med. 2020;39:519–530. doi: 10.1016/j.accpm.2020.06.016.
-
Gopinath R, Ayya SS. Neurogenic stress cardiomyopathy: what do we need to know. Ann Card Anaesth. 2018;21:228–234. doi: 10.4103/aca.ACA_176_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
-
Chen Z, Venkat P, Seyfried D, Chopp M, Yan T, Chen J. Brainheart interaction: cardiac complications after stroke. Circ Res. 2017;121:451–468. doi: 10.1161/CIRCRESAHA.117.311170. [DOI] [PMC free article] [PubMed] [Google Scholar]
-
Biso S, Wongrakpanich S, Agrawal A, Yadlapati S, Kishlyansky M, Figueredo V. A review of neurogenic stunned myocardium. Cardiovasc Psychiatry Neurol. 2017;2017:5842182. doi: 10.1155/2017/5842182. [DOI] [PMC free article] [PubMed] [Google Scholar]
-
Lee VH, Oh JK, Mulvagh SL, Wijdicks EF. Mechanisms in neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2006;5:243–249. doi: 10.1385/NCC:5:3:243.
-
Robba C, Bonatti G, Pelosi P, Citerio G. Extracranial complications after traumatic brain injury: targeting the brain and the body. Curr Opin Crit Care. 2020;26:137–146. doi: 10.1097/MCC.0000000000000707. [DOI] [PubMed] [Google Scholar]
-
Dantzer R, Konsman JP, Bluthé RM, Kelley KW. Neural and humoral pathways of communication from the immune system to the brain: parallel or convergent? Auton Neurosci. 2000;85:60–65. doi: 10.1016/S1566-0702(00)00220-4.
-
Kerro A, Woods T, Chang JJ. Neurogenic stunned myocardium in subarachnoid hemorrhage. J Crit Care. 2017;38:27–34. doi: 10.1016/j.jcrc.2016.10.010.
-
Krishnamoorthy V, Mackensen GB, Gibbons EF, Vavilala MS. Cardiac dysfunction after neurologic injury: what do we know and where are we going? Chest. 2016;149:1325–1331. doi: 10.1016/j.chest.2015.12.014.
-
Havakuk O, King KS, Grazette L, Yoon AJ, Fong M, Bregman N, et al. Heart failure-induced brain injury. J Am Coll Cardiol. 2017;69:1609–1616. doi: 10.1016/j.jacc.2017.01.022. [DOI] [PubMed] [Google Scholar]
-
1Claassen JAHR, Thijssen DHJ, Panerai RB, Faraci FM. Regulation of cerebral blood flow in humans: physiology and clinical implications of autoregulation. Physiol Rev. 2021;101:1487–1559. doi: 10.1152/physrev.00022.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
-
Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017;60:1–12. doi: 10.1016/j.bbi.2016.03.010.
-
Hoogland IC, Houbolt C, van Westerloo DJ, van Gool WA, van de Beek D. Systemic inflammation and microglial activation: systematic review of animal experiments. J Neuroinflammation. 2015;12:114. doi: 10.1186/s12974-015-0332-6. [DOI]
-
Ziaka M, Exadaktylos A. Brain-lung interactions and mechanical ventilation in patients with isolated brain injury. Crit Care. 2021;25:358. doi: 10.1186/s13054-021-03778-0.
-
de Gregorio C. Cardioembolic outcomes in stress-related cardiomyopathy complicated by ventricular thrombus: a systematic review of 26 clinical studies. Int J Cardiol. 2010;141:11–17. doi: 10.1016/j.ijcard.2009.09.468.
-
Kenigsberg BB, Barnett CF, Mai JC, Chang JJ. Neurogenic stunned myocardium in severe neurological injury. Curr Neurol Neurosci Rep. 2019;19:90. doi: 10.1007/s11910-019-0999-7.
-
Porto I, Della Bona R, Leo A, Proietti R, Pieroni M, Caltagirone C, et al. Stress cardiomyopathy (tako-tsubo) triggered by nervous system diseases: a systematic review of the reported cases. Int J Cardiol. 2013;167:2441–2448. doi: 10.1016/j.ijcard.2013.01.031.
-
Sposato LA, Fridman S, Whitehead SN, Lopes RD. Linking stroke-induced heart injury and neurogenic atrial fibrillation: a hypothesis to be proven. J Electrocardiol. 2018;51:430–432. doi: 10.1016/j.jelectrocard.2018.02.006. [
-
Sposato LA, Hilz MJ, Aspberg S, Murthy SB, Bahit MC, Hsieh CY, et al. Post-stroke cardiovascular complications and neurogenic cardiac injury: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76:2768–2785. doi: 10.1016/j.jacc.2020.10.009. [DOI] [PubMed] [Google Scholar]
-
Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, et al. Clinical features and outcomes of takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373:929–938. doi: 10.1056/NEJMoa1406761. [
-
Scheitz JF, Nolte CH, Doehner W, Hachinski V, Endres M. Stroke-heart syndrome: clinical presentation and underlying mechanisms. Lancet Neurol. 2018;17:1109–1120. doi: 10.1016/S1474-4422(18)30336-3.
-
Ogren JA, Fonarow GC, Woo MA. Cerebral impairment in heart failure. Curr Heart Fail Rep. 2014 Sep;11(3):321-9. doi: 10.1007/s11897-014-0211-y. PMID: 25001614.
-
Pelliccia F, Kaski JC, Crea F, Camici PG. Pathophysiology of takotsubo syndrome. Circulation. 2017;135:2426–2441. doi: 10.1161/CIRCULATIONAHA.116.027121.
-
Balint B, Jaremek V, Thorburn V, Whitehead SN, Sposato LA. Left atrial microvascular endothelial dysfunction, myocardial inflammation and fibrosis after selective insular cortex ischemic stroke. Int J Cardiol. 2019;292:148–155. doi: 10.1016/j.ijcard.2019.06.004. [DOI] [PubMed] [Google Scholar]
-
Suzuki H, Matsumoto Y, Kaneta T, Sugimura K, Takahashi J, Fukumoto Y, et al. Evidence for brain activation in patients with takotsubo cardiomyopathy. Circ J. 2014;78:256–258. doi: 10.1253/circj.cj-13-1276.
-
Masuda T, Sato K, Yamamoto S, Matsuyama N, Shimohama T, Matsunaga A, et al. Sympathetic nervous activity and myocardial damage immediately after subarachnoid hemorrhage in a unique animal model. Stroke. 2002;33:1671–1676. doi: 10.1161/01.str.0000016327.74392.02.
-
Prosser J, MacGregor L, Lees KR, Diener HC, Hacke W, Davis S, VISTA Investigators Predictors of early cardiac morbidity and mortality after ischemic stroke. Stroke. 2007;38:2295–2302. doi: 10.1161/STROKEAHA.106.471813.