Sense of balance
Balance disorders and dizziness
The brain
Introduction
After sustaining a brain injury, many people report experiencing balance problems, vertigo, and/or unsteadiness of movement. Even in people without a brain injury who experience balance problems, the brain can be "out of balance" and cause numerous symptoms.
Symptoms can range in severity from mild to disabling.
There are so many factors involved in maintaining balance or avoiding dizziness that we hope the information on this page won't make anyone dizzy.
You can also read the summary of this page via this link!
Balance problems are not always accompanied by dizziness. Dizziness is always accompanied by a loss of balance to a greater or lesser extent.
Balance is the ability to center the body on its support point (fulcrum). When walking or standing, the feet serve as the fulcrum. If someone uses a cane or a walker, the assistive device provides an additional fulcrum. When someone sits, the buttocks, thighs, and feet provide the fulcrum. If someone leans against something, another fulcrum is added. If the fulcrum moves significantly, such as with a boat, skateboard, surfboard, or similar device, maintaining balance becomes much more difficult.
If someone has a disease of the balance organ (vestibular organ), there may also be problems when lying, sitting or leaning on the support point.
Topics on this page are divided into:
1) What is balance and the sense of balance?
2) What is needed to maintain balance?
- The vestibular organs are important.
- Reflexes are important.
- Brain areas are important:
- Muscles and proprioception are important:
3) What can go wrong with balance, for example, due to injury or illness?
- Influence of visual problems (problems with seeing) on balance
- The influence of poor movement on balance
- The influence of other factors on balance
- Acute brain injuries and balance
4) Diseases of the vestibular system
Diseases of the vestibular system
What constitutes balance?
Static balance
The ability to maintain balance while not moving.
Dynamic balance
The ability to maintain balance while moving.
The ability to maintain balance while performing multiple tasks simultaneously, such as talking and doing something.
The sense of balance
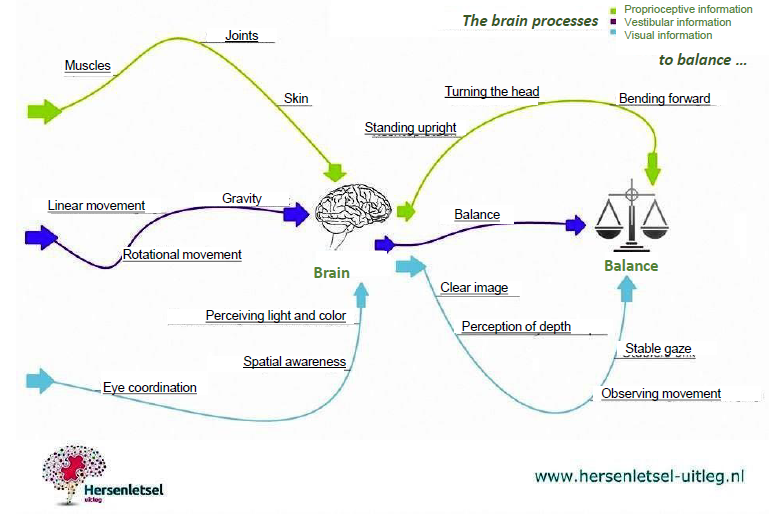
The sense of balance is determined by information from:
- positional sense or proprioception, which uses muscles, joints, tendons, connective tissue, and skin to sense the body's position. This is necessary for sensing what is happening.

- vision/eyes, visual perception
This is necessary to see what is happening.

- The vestibular organ. This organ is necessary for sensing gravity, what is up and what is down, and for sensing whether you are moving or if your surroundings are moving. It also provides orientation in space and helps maintain postural stability and balance.

Every human being has a balance organ on each side of their head: in the inner ear, behind the eardrum, and behind the temporal bone.
Both balance organs, in the left and right ear, are necessary for postural balance, spatial orientation, and image stabilization.
The balance organ, together with the cochlea of the ear, forms the labyrinth.
The balance organ consists of:
1) The semicircular canals in the inner ear. They contain gelatinous fluid: perilymph and endolymph. This gelatinous mass rests on sensory hairs, tiny hair cells (sensors) that track the rotation of the head. They register rotational movements in different directions.
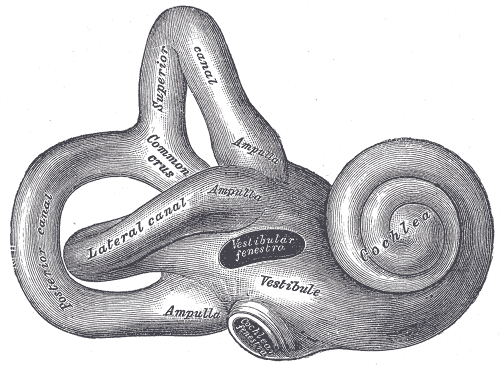
The three semicircular canals are shown on the left side of the image. The vestibular organ (the organ of balance), named after "the vestibule," is in the center of the image.
Image from Gray
2) The otolith organ registers the linear acceleration (forward or backward) of the body. This allows the position relative to gravity to be determined, as well as posture in various horizontal directions.
The otolith organs consist of the saccule and the utricle.
Otos is the Greek word for ear and lithos for stone. The otolith organs contain crystals (statoconia). Due to their inertia, these crystals lag behind the acceleration of the head during movement. Thus, they play a role in the perception of acceleration, movement, and gravity.
In the video below, you can clearly see how the three semicircular canals are activated by different head movements. This way, you can also diagnose dizziness only with certain head movements by identifying which canal has a detached crystal. People with BPPV, or Benign Paroxysmal Positional Vertigo, suddenly experience this dislodged crystal. And that suddenly makes you very ill.
Image Stabilization through Reflexes
1) Vestibulo-Ocular Reflex (VOR)
The vestibular system "senses" head movements and can counter-steer the eyes through image stabilization to maintain sharp vision even during the fastest movements. This occurs via the fastest motor reflex, the vestibulo-ocular reflex (VOR). This reflex lasts only eight milliseconds. The word "vestibular" refers to the vestibular system and comes from the vestibule (the entrance to the inner ear). The word "ocular" comes from the Latin word oculus, meaning eye.
When someone looks at something and wants to keep looking at it, this is what happens when they move their head: If they move their head to the left, their eyes move to the right, and vice versa, as do sideways and top-down movements. The eyes move in the opposite direction to the head, while the person remains focused on a single fixed point.
If this reflex is disturbed, the person will become dizzy, the world will seem to tilt, and they may lose their balance. They may see vibrating images.
2) Cervico-ocular reflex (COR)
The interaction between the vestibular system and the eyes is called the vestibulo-ocular reflex (VOR). However, there is another important reflex: the one between the neck and the eyes. This reflex is called the cervico-ocular reflex (COR). The word 'cervico' refers to the neck (cervix). The word 'ocular' comes from the Latin word oculus, meaning eye. It is a stabilization reflex of the eyes when the neck is turned.
If a disruption occurs in the cervico-ocular reflex, a person may experience impaired vision, dizziness, and lightheadedness. This can occur, for example, with a neck injury such as whiplash.
The cervico-ocular reflex appears to be able to make a valuable contribution to the diagnosis of cervical trauma such as whiplash.
This reflex can be elicited by turning the neck in the absence of vestibular (balance) or visual (eye) stimuli. This means that the body is turned in the dark, with a fixed head.
3) Optokinetic Reflex (OKR)
The cervico-ocular reflex works naturally with the vestibulo-ocular reflexes to stabilize the image on the retina during movement.
The optokinetic reflex returns the eyes to their initial position when a person follows a moving object that moves out of their field of vision.
The influence of the brainstem and cerebellum on balance
Information from the vestibular system is transmitted to the cerebellum.
One specific area in the cerebellum that is important for balance is called the vestibullocerebellum.

This area regulates many aspects of maintaining balance:
- coordination of movement
- balance and equilibrium
- memory for reflex motor actions / regulation of reflexes
- oculomotor function
- muscle tone
- integration of tactile and deep sensory stimuli.
People with cerebellar injuries may therefore experience balance problems.
With the cerebrum, a person becomes aware of this information. In most cases, these are unconscious, automatic processes.
The brainstem has three areas.

1. The pons: balance, body position/posture, and muscle tension.
2. The mesencephalon (midbrain): Information from the eyes is processed, and a reflex occurs when necessary. It regulates muscle tension and posture. It produces dopamine.
This is important for the body to be able to make movements. Without dopamine, a person cannot correct the muscles to prevent a fall.
3. The medulla oblongata regulates heart rate and blood pressure (cardiovascular function). A constant supply of blood to the brain through the correct blood pressure plays an important role in maintaining balance.
This is also where breathing and control of the respiratory muscles are regulated, and carbon dioxide and oxygen levels in the blood are detected. All of this is necessary for maintaining balance. If you have too much or too little oxygen in your blood, you become lightheaded or dizzy.
If the balance organ sends the "wrong" information, the brain may misinterpret body movements. People with lesions in the cerebellum or the brainstem may therefore experience balance problems.
The influence of muscles on balance
The cerebellum and brainstem control the body's muscles to make adjustments to maintain balance, prevent falls, and remain stable. The brain coordinates these movements.
People with muscle problems are therefore more likely to fall.
The Influence of Proprioception on Balance
Sensory cells in muscles, joints, tendons, connective tissue, and skin transmit information to the sensory nerves. This information reaches the cerebellum via the spinal cord, where it processes information from the three senses of balance (vision, proprioception, and equilibrium).
This is how the brain senses how the body is positioned in relation to the space around it. These sensors form the proprioceptive sense.
When something is wrong with proprioception, a person loses balance and may experience lightheadedness, dizziness, or the sensation that the world is moving.
Brain areas that help with spatial orientation, enable movement, and balance
Last but not least, are the brain areas that help with spatial orientation and enable movement. If these areas are damaged by a brain injury, it can affect balance.
Enabling movement
The basal ganglia contains several nuclei that (partly) regulate balance, posture, eye movements, and the initiation of movement. In adults, postural reflexes are stored here.
Both the thalamus and the motor cortex are crucial for motor function.
Spatial Orientation
The following brain areas are part of the network involved in spatial orientation:
- the right hemisphere
- the frontal lobes
- the parietal lobe
This last lobe, like the vestibular system, signals which way is up. It is therefore part of our spatial orientation. It prevents us from bumping into things.
The central part of this lobe primarily controls gross motor skills (legs and limbs).
Together, they ensure that a person can adjust their posture and maintain balance.
Motor Memory
"Motor memory" may be lost due to a brain injury. Normally, it ensures the proper coordination of movements, without the involvement of conscious memory. This results in "incorrect" signals being sent that can be misinterpreted. The person may become unsteady on his or her feet.
People with injuries to these brain areas may therefore experience balance problems.
Blood pressure, blood flow, blood sugar levels, alcohol, and medication are important for balance
The following factors can significantly impact balance.
Correct blood pressure
A constant supply of blood to the brain through correct blood pressure plays a crucial role in maintaining balance.
Blood pressure and heart rate are considered "autonomic functions"; functions you cannot influence with your will. They function "autonomously."
In case a person becomes dizzy upon standing, has blurred vision, sees black spots, or nearly falls, she or he may have orthostatic hypotension.
This literally means a drop in blood pressure after standing. Orthostatic means "upright posture."
Sometimes the term "postural hypotension" is used. Postural then means posture-dependent.
The blood vessels don't constrict enough, and the heart rate doesn't increase sufficiently to stimulate the body to action. This can also happen when someone rises from a lying position to a sitting position. Causes can include blood loss, dehydration (not drinking enough fluids), infection, medication (water pills or antidepressants), and chronic alcoholism. Even a hot bath or shower, or a neurological condition, can be a cause.
All these causes involve either the blood vessels being too dilated or insufficient blood volume.
Autonomic Function Damage
If, due to a brain injury or concussion,
the autonomic nerves—the nerves that control organs like the heart, lungs, and blood vessels—don't function properly, this can cause dramatic fluctuations in blood pressure, resulting in dizziness and a tendency to faint.
Examples include the conditions Postural Orthostatic Tachycardia Syndrome (POTS) and orthostatic hypotension (OH). These are classified as dysautonomia.
Cardiac Arrhythmias
Cardiac arrhythmias may cause dizziness.
A circulatory disorder or bleeding in the vestibular system and/or (cerebral) brain may cause dizziness.
Blood Sugar Levels
Low blood sugar levels may significantly impact dizziness.
Medications
Some medications may cause dizziness.
Alcohol
Alcohol use may also lead to a light-headed feeling or, more seriously, an inability to maintain balance.
Kink in the Cable
It's important for balance that everything in the body functions properly. To maintain good equilibrium,
the ears, the two organs of balance, eyes, muscles, blood pressure, heart rate, breathing, and brain function are particularly important.
It's also crucial that these factors work well together.
If even one function or organ isn't functioning properly, the body must compensate with other functions and organs.
In each of these processes, the brain injury can cause a glitch, leading to dizziness or unsteadiness. A person may feel like the world is moving, experience lightheadedness, stumble, and stagger. A person may no longer be able to quickly correct themselves to avoid falling. Furthermore, a person may experience severe nausea, vomiting, or even fainting.
However difficult it may be, it is important to diagnose whether damage has occurred in the balance organ, the eyes or the connection between eyes and balance, the muscles and their control, deproprioception, heart rate and blood pressure regulation, or any of the brain areas or how they work together, or whether an acute cerebral hemorrhage or cerebral infarction (stroke) has occurred.
Acute Brain Injury
If you experience acute dizziness this can be a sign of a stroke. An acute stroke can cause acute dizziness and imbalance. This may include vertigo, nausea, with or without vomiting. There may be an intolerance to head movements, which can be accompanied by imbalance.
Read about the warning signs that someone may have suffered a cerebral hemorrhage, cerebral infarction, or transient ischemic attack (TIA) via this link.
Other acute brain injuries and chronic phase brain injuries can also cause balance problems.
Poor vision due to a brain injury may affect balance
Everyone will recognize that in the dark, you can lose your balance more easily and lose your bearings. Closing your eyes makes walking or standing still more difficult. If there's a problem with your eyes or the visual system in your brain, balance can be completely lost.
Many visual problems can occur due to brain injury. All symptoms may affect balance or cause dizziness. We list a few here:
- Eye movement disorders
- Gaze paralysis (gaze palsy)
- Eyelid spasm (blepharospasm)
- CVI problems: cerebral visual disturbances, with fluctuating visual acuity
- Half-sided visual field loss: hemianopia
- Double vision (diplopia)
- Refractive error: inability to focus
- Unable to perceive something on half a side due to (hemispatial) neglect, may lead to bumping into objects or hitting objects
- Fixation disparity problems: each eye receives an image, which is sent to the brain via the optic nerves. There, these two images are combined into a single image. If this is no longer possible due to brain injury, it is called a 'fixation disparity problem'.
- Pathological nystagmus (eye wobble, back and forth, up and down, or rolling), characterized by:
- eye movement back and forth
- seeing a vibrating image
- reduced visual acuity
A person with nystagmus often suffers from dizziness.
Pathological nystagmus may occur due to nervous system disorders (congenital or acquired), sleep deprivation, medications, alcohol, balance disorders or circular movements.
Nystagmus may also be a normal phenomenon when the semicircular canals register angular acceleration and then send signals to the eye movement nuclei in the brain.
Nystagmus also occurs when the semicircular canals are stimulated while the head is stationary.
Being unable to move properly due to a brain injury may affect balance

In case an imbalance is registered in the brain, the vestibular system, or with the eyes, but the muscles cannot adjust, a person may quickly lose balance.
Here are some problems that may arise after a brain injury:
- Half-sided paralysis (left or right)
- Loss of muscle strength (either on one side or not; paresis)
- Movement disorder
- Upper motor neuron damage with spasm or spasticity
- Damaged sensory nerves
- Combination of postural problems due to damage to the basal ganglia (parkinsonism): decreased movement (hypokinesia), slowed movements (bradykinesia), impaired posture, postural deviation, impaired postural reflexes, loss of postural reflexes, and stiff limbs
- Ataxia: impaired movement due to damage to the cerebellum
- Damage to a part of the thalamus may lead to sensory disturbances in the opposite side of the body and can also cause movement disorders, a lack of movement (motor disorders). This can lead to loss of balance. Injuries to the thalamus can also lead to visual field loss. As this page describes, the eyes are one of the most important pillars of balance.
Diseases of the balance organ

In case something is wrong with the balance organ, intense dizziness may occur. Acute attacks of vertigo can completely paralyze life. It can be very frightening, along with all the physical symptoms of nausea, vomiting, drop attacks, and fainting.
The function of one of the balance organs may suddenly fail due to, for example, an infection or trauma. This results in vertigo.
This is seen, for example, in vestibular neuritis.
Recurring episodes of vertigo - lasting minutes to days - can also occur, such as in BPPV (see below), Ménière's disease, or vestibular migraine.
Furthermore, damage to one or both balance organs can result in a constant feeling of imbalance.
A blow, a fall, or a collision, for example, due to traumatic brain injury, an infection, or aging, can dislodge the ear stones and cause them to end up in the other part of the balance organ: the fluid (perilymph) of the semicircular canals.
Balance is then immediately lost and the person may become very ill and vomit. The eyes may wobble or make rapid jerking movements (nystagmus).
Only when the fluid has stopped spinning will the intense spinning sensation and the feeling of seasickness subside.
ople with a balance disorder can be severely limited in their working and social lives. They can quickly and severely become overstimulated, leading to new symptoms.
Sudden (spinning) dizziness
- Vestibular neuritis is an inflammation of the vestibular nerve. Because the symptoms are not always associated with an infection this condition is called acute vestibular dysfunction.
Vestibular neuritis is characterized by persistent, rotating dizziness for several days, accompanied by nausea. People with acute vestibular dysfunction are generally seriously ill due to the severe dizziness and nausea and prefer to remain in bed for the first few days.
Sometimes the auditory nerve is also inflamed, and hearing loss/deafness (labyrinthitis) also occurs. For most people, the symptoms diminish over the course of days to weeks. A small group continues to experience symptoms for much longer.
Labyrinthitis is often mentioned in the same breath as vestibular neuritis, and vice versa, but the difference lies in the hearing loss that occurs with labyrinthitis. The symptoms of vertigo are the same with vestibular neuritis (above) as with labyrinthitis (below).
- Labyrinthitis is an inflammation of the labyrinth, which contains the three semicircular, fluid-filled canals. The labyrinth is the combined ear and balance organ.
It is characterized by persistent vertigo for several days, accompanied by nausea. People with acute loss of balance are generally seriously ill due to the severe dizziness and nausea and prefer to remain in bed for the first few days. The symptoms of vertigo are the same with vestibular neuritis as with labyrinthitis, but hearing loss also occurs with labyrinthitis.
- Acute brain injuries, such as a stroke, a cerebral hemorrhage, a dissection (rupture) of blood vessels, traumatic brain injury after an accident, a blow, mistreatment, or damage to the labyrinth due to a stroke, infection, or trauma.
Recurrent (spinning) dizziness
- Positional vertigo, or benign paroxysmal positional vertigo (vertigo) (BPPV), is caused by dislodged ear stones. Benign means non-cancerous. Paroxysmal means "attack-like." Vertigo is spinning dizziness.
Characteristic are short-lived attacks of spinning vertigo with imbalance caused by sudden changes in the head position, such as bending over and sitting up, turning in bed, looking up, or turning the neck or trying to look backward. The diagnosis is confirmed with a tilt test. Vertigo attacks are very brief, lasting about a minute or a little longer. However, some people, especially older adults, may experience a constant wobbly feeling. BPPV is often confused with PPPD (the first "P" stands for "Persistent").
It sometimes happen that someone experiencing vertigo caused by BPPV/V experiences nausea, vomiting, fainting, visual disturbances, or severe neck pain. The latter is due to increased tension in the neck muscles.
These are rare situations.
Treatment: Doing the Epley maneuver may help.
A video about the Epley Maneuver
- Benign recurrent vertigo, also called recurrent vestibulopathy, is characterized by sudden attacks of rotating dizziness without hearing loss. The symptoms may disappear on their own. In some cases, the condition persists and can then lead to hearing loss. In some cases, the condition persists and can then lead to hearing loss. The condition then appears to be a form of Ménière's disease.
- Vestibular schwannoma is a tumor in the Schwann cell, the sheath and the supporting cell of the eighth cranial nerve (vestibulocochlear nerve). This nerve carries information about sound and equilibrium from the inner ear to the brain. Most people with a vestibular schwannoma experience unilateral hearing loss and a feeling of unsteadiness when walking (balance disorder). See our more detailed information about vestibular schwannoma.
- Cardiovascular dizziness
Characteristic are attacks of symptoms accompanied by palpitations or a fast or slow heart rate.
- Cervicogenic dizziness
This type of dizziness is neck-related and is triggered by neck movements. It may be caused by the position of the cervical vertebrae and head, increased muscle tension, an accident or poor circulation, for example, due to osteoarthritis.
The proprioception muscle spindles may send incorrect, impure, or unknown signals from the neck to the brain, which may also cause dizziness.
Degenerative changes in the seven cervical vertebrae may lead to neurovascular compression. This causes, in addition to stiffness, irritation of nerve pathways in the neck. Pain is often felt in the neck or back of the head, with radiating pain behind the eyes. The person may be unsteady on their feet, feel lightheaded or unstable, and prefer to sit down. She or he may be sensitive to cold, experience chills, and feel tension in the neck. The symptoms may become chronic.
- DFNA9 is an autosomal dominant progressive sensorineural hearing loss, often starting in the age of forty (in some cases much earlier) with periods of severe dizziness accompanied by vegetative symptoms (sweating, nausea, pallor, restlessness, or anxiety).
It is striking that the hearing loss does not occur in both ears simultaneously. One ear may become hearing impaired faster than the other.
- Hyperventilation syndrome is characterized by dizziness with tingling fingers, tingling around the mouth, or chest pressure. It may be accompanied by sweating, restlessness, and/or anxiety.
It is caused by a breathing disorder. Breathing occurs too rapidly, resulting in the exhalation of too much carbon dioxide (CO2).
- MdDS (Mal de débarquement Syndrome)
This is a condition characterized by a subjective perception of self-motion. It produces a rocking (boat-like) sensation when sitting still or
while standing or moving from one position to another. The persistent (continuous) sensation of movement is described as rocking, swaying, tumbling, and/or hopping after a period of passive movement, such as after sailing or traveling by train, car, or plane, but sometimes also other movements (such as sleeping on a waterbed). It produces a foggy, fuzzy feeling in the head.
It is striking that movement makes people feel better than sitting still, standing still, or lying down, which can cause discomfort.
- Superior canal dehiscence syndrome SCDS is an inner ear disorder that can cause dizziness due to sound and pressure changes.
It causes vertigo with vibrating images or blurred vision during triggers.
People experience the sensation of objects moving in their visual field (oscillopsia) when hearing sound or when pressure changes in the affected ear.
It causes a feeling of imbalance.
- PPPD (Persistent Positional Perceptual Dizziness) (Triple PD) is a nearly constant, persistent feeling of dizziness and a sensation of swaying, influenced by body position and movement.
This condition encompasses several symptoms, including chronic subjective dizziness and visual vertigo.
The symptoms can last for hours, but are not necessarily constant. They can vary in severity. PPPD is preceded by conditions that cause vertigo, imbalance, or dizziness. These include acute vestibular syndromes, episodic or chronic vestibular syndromes, neurological disorders, brain injuries, and psychological conditions.
- Bilateral Vestibulopathy (BVP)
The symptoms of this condition may vary in severity. Balance disorders are characteristic, particularly during walking. The symptoms of unsteadiness while walking increase in the dark, as the eyes can no longer compensate. A person may have difficulty walking on uneven surfaces. An unsteady feeling in the head is often reported, as is a blurred, vibrating vision (oscillopsia) during movement. Spatial memory is often impaired.
The symptoms are particularly present during movement.
There are many possible causes. BVP can result from trauma to the temporal bone (os temporale), a stroke, a cerebral hemorrhage, meningitis, Borrelia, Creutzfeldt-Jakob disease, CANVAS (Cerebellar Ataxia with Neuropathy and bilateral Vestibular Areflexia Syndrome), other neurodegenerative diseases that occur simultaneously with shrinkage of the cerebellum and/or polyneuropathy), an autoimmune condition such as rheumatoid arthritis, lupus erythematosus, vasculitis, or bilateral Meniere's disease, antibiotic use (in 30% of cases!) such as gentamicin, tobramycin, and streptomycin, and to a lesser extent vancomycin, vitamin B12 deficiency, two hereditary forms of deafness (DFNA9 and DFNA11), and other unknown disorders.
- Vestibular Migraine: multiple attacks of severe vertigo, lasting minutes to hours, up to three days. A history of migraine and migraine symptoms are present in more than half of the vertigo attacks. The person has an erroneous sensation of movement or that the world is moving.
Migraine symptoms include: hypersensitivity to light and sound, seeing spots or flickering (scotomas) before the eyes, a visual aura, flashes of light, and headaches with nausea or vomiting. Note: a migraine headache is not always present!
Vestibular Paroxysms (VP)
This condition involves a so-called neurovascular conflict. A blood vessel may compress the eighth cranial nerve (the nerve responsible for hearing and balance).
It is characterized by recurrent, brief attacks of vertigo that can last seconds to minutes. This can occur several times a day. The attacks can occur spontaneously, triggered by hyperventilation, or after moving the head. It is sometimes difficult to distinguish from benign paroxysmal positional vertigo (BPPV). Sometimes the symptoms are accompanied by brief tinnitus and hearing loss.
Vestibular Schwannoma See also: cerebellopontine angle tumor
Meniere's syndrome is a disorder of the inner ear. Both inner ears contain the cochlea and the organ of balance.
In Meniere's syndrome, the underlying cause for all three symptoms is known (for example, a cerebellopontine angle tumor). In Meniere's disease, the cause is unknown.
See also this information about the difference between Meniere syndrome or Meniere Disease
The condition is characterized by attacks of vertigo lasting at least 20 minutes and up to 12 hours, ringing in the ears (tinnitus), a feeling of fullness in the affected ear, and an audiometrically determined hearing loss of at least 30 dB in the low- to mid-range frequencies.
Vertigo is a sensation that the world is spinning or that the person is spinning. The attack occurs without any apparent cause, although some people report certain triggers. Hearing loss can fluctuate early in the disease.
The feeling of pressure in the ear or a feeling of fullness is caused by excess pressure in the membranous part of the inner ear. This excess pressure is called endolymphatic hydrops.
This excess pressure is damaging to the hearing organ. The excess fluid pressure can rupture the wall of a compartment in the cochlea, mixing two different substances (endolymph and perilymph), which likely triggers the vertigo attack.
A person may experience nausea, which may or may not be accompanied by vomiting. The patient may look pale and have 'cold sweats'.
Usually, one ear is affected, but probably both ears are affected in a third of people with these symptoms. The hearing loss is initially temporary and eventually becomes permanent. Sometimes it can be so severe that the ear becomes completely deaf.
An attack may be brief, lasting about 20 minutes, or even last up to 12 hours. Attacks can occur infrequently or recur weekly. Some people experience multiple attacks a month or only twice a year.
Attacks can occur suddenly, but as the patient becomes more familiar with the condition, they are often heralded by ear problems.
As a result of the attacks, damage occurs to the affected balance organ, and people experience an unstable feeling between attacks (unilateral or bilateral vestibulopathy).
Patients often report visual symptoms (visually induced vertigo, visual hypersensitivity, visual vertigo, visually induced dizziness). This is due to overload of the ears, balance organ, eyes and brain, as these organs work so closely together.
The visual symptoms may lead to (visual) sensory overload. In people without brain damage, these are very similar to those experienced by people with brain damage, because the brain is functionally overloaded during a seizure.
Vision may deteriorate because the vestibular system is responsible for image stabilization (that is, keeping the image steady when the head moves). This impairment may cause the image to move up and down when walking or moving. A person may also experience blurred vision while moving; focusing becomes more difficult when moving the head. This is called oscilopsia.
Over the years, the vertigo attacks almost always subside. The Ménière's disease then fades. The residual damage to hearing and balance remains. The extent of this damage varies from person to person and may also vary from ear to ear. Tinnitus may also be permanent. Most people also experience persistent hyperacusis and (visual) overstimulation symptoms due to the excessive strain on their balance organs.
A small percentage of Meniere's patients experience drop attacks.
They are also called otolithic crises, Tumarkin drop attacks, or vestibular attacks. The person falls to the ground without warning, as if pushed over.
There is no loss of consciousness or neurological symptoms. These can be very frightening experiences, as no one knows when the attack might occur.
See the download for the clinical study on these drop attacks.
More information can be found on the following websites: