Headache
Shortcut menu
- headache after stroke
- headache after traumatic brain injury
- headache due to whiplash
- headache caused by CCI/AAI
- headache due to cerebral edema
- headache caused by overstimulation
- headache by heat / dehydration
- trigeminal / facial pain
- tension headache
- headache from the neck / cervicogenic headache
- supra orbitalis neuralgia
- withdrawal headache / rebound
- migraine
- cluster headache / chronic cluster headache
- SUNCT headache
Headache is one of the most frequently mentioned complaints after brain injury. More than 41% of people with different types of brain injury have headache complaints in the first year.
Acute phase and chronic phase
Immediately after a brain trauma, the headache may be caused by the scar, by blood clots that still provide pressure and by fluid in the brain.
Headache that occurs for a long time after the injury can occur, among other things, due to the change in the brain structure due to the injury, injury in the neck and skull, due to stress and tension, due to overload, neurofatigue, overstimulation and it can even be caused by medication.
Headaches may come and go. They may completely affect someone's functioning, for example cognitively.
Not everyone is left with a headache as a residual symptom.
Stroke and headache
Chronic headache is estimated to occur in 10% of patients after a stroke. Headache in the early period of a stroke is a predictor of headache six months after a stroke. People with a history of tension headaches or vascular headaches are more likely to develop headaches after a stroke. (Vascular headache is an outdated term used to refer to certain types of headaches, including migraines, cluster headaches, and fever associated with another condition.)
The cause of headaches after a stroke is not fully known. The stimulation of nerve cells in the fifth cranial nerve (trigeminal nerve) is one possibility. These nerve cells (neurons) ensure the contraction or dilation of the cerebral blood vessels (trigeminovascular system).
The damage or changes to the blood vessels and the subsequent inflammation or disruption and/or stimulation of pain pathways could be a cause.
Traumatic brain injury and headache
Migraine-like headaches are noted in both mild and severe traumatic brain injury, as well as in patients with whiplash injuries. NB! Not everyone has a headache! Immediately after a brain trauma, the headache may be caused by the scar, by blood clots that still provide pressure and by fluid in the brain.
In addition to headaches, pain in the neck is also frequently mentioned. See also the paragraph cervicogenic headache (headache from the neck).
Particularly in people with severe traumatic brain injury, but also patients with whiplash or mild traumatic brain injury such as concussion. It must be ruled out whether someone has a neck hernia or broken neck. Even after years, people report having daily headaches.
Pain in the neck due to whiplash
Neck pain and headaches are two of the most common complications of whiplash injuries. One study showed that an average of 60% had headaches within seven days after a whiplash injury. Twelve months after the whiplash injury, an average of 38% of patients still had neck pain.
See also the paragraph cervicogenic headache (headache from the neck). Read more on the page whiplash/WAD.
Headache by CCI/AAI
CCI refers to instability in the area where the skull and upper cervical vertebrae meet, while AAI involves instability between the first and second cervical vertebrae (atlas and axis). See also this page.
Headache due to cerebral edema /
Idiopathic Intracranial Hypertension (IIH)
Headache due to cerebral artery pressure syndrome, also known as a cerebrospinal fluid pressure problem in the spinal cord and brain, is a condition in which the pressure in the brain is not properly regulated.
Headaches from cerebral edema occur when fluid builds up around the brain, leading to increased intracranial pressure.
Cerebral pressure is also called intracranial pressure or ICP. More information can be found here and here.
Headache due to overstimulation
There is also a headache that occurs after cognitive or sensory overstimulation.
The headache occurs almost immediately when a person receives more stimuli than he or she can process.
We distinguish the following forms of overstimulation:
- Cognitive overstimulation
The environment demands too much of the brain. Pace, workload, executive functions, thinking tasks or emotions are no longer (properly) processed. Everything feels like too much, too busy, concentration is difficult and overview is lacking.
- Sensory overstimulation
Caused by stimuli via the senses, such as background noise, noise, seeing light, interrupted light, movements, colours, patterns, touch, temperature, smells, posture and position sense (proprioception).
Headache from heat or dehydration
As a result of brain damage, heat intolerance or problems with temperature regulation can occur. We have a separate page about that.
If the temperature cannot be regulated properly by the brain, a person can experience headaches.
Headaches can always be a result of heat or dehydration, especially on hot days or during physical exertion. When the body loses too much fluid and minerals, for example through sweating, this can lead to dehydration. This disrupts the balance in the body and can cause headaches.
Heat can also be a direct trigger, because the blood vessels expand to cool down, which can put pressure on the nerves in the head.
Trigeminal neuralgia / Facial pain
This form of facial pain can have various causes. Brain injury is not always the cause.
A stroke or traumatic brain injury can cause trigeminal neuralgia (facial pain or tic douloureux).
Especially with damage in the brain stem or damage with damage to one of the nerve branches, usually with pain on one side of the face. Fractures in the skull, from a fall or a car accident can cause swelling that damages the nerve. Injuries to soft tissue can sometimes only affect one or two branches of the nerve, so that the rest of the face has no pain.
There are also known cases in which a stroke, often a cerebral infarction in the brain stem, causes symptoms that are very similar to the pain of trigeminal neuralgia (TN). That pain has a good prognosis. Sometimes it happens the other way around: Pain that resembles trigeminal neuralgia can be a warning sign of a stroke in the brain stem (medulla or medulla oblongata).
Known causes
- Sometimes blood vessels in the area around the cranial nerve swell or an artery near the trigeminal nerve presses against this nerve. This may also happen because the heartbeat exerts pressure, which makes the nerve extra sensitive. As a result, even small touches to the face can cause severe pain.
- A stroke or traumatic brain injury can also cause trigeminal neuralgia (facial pain or ticdouloureux). Especially with damage in the brainstem or damage that affects one of the nerve branches, usually with pain on one side of the face. Fractures in the skull, from a fall or a car accident can cause swelling that damages the nerve. Soft tissue injuries can sometimes only affect one or two branches of the nerve, so that the rest of the face has no pain.
- There are also cases in which a stroke, often a cerebral infarction in the brainstem, causes symptoms that closely resemble the pain of trigeminal neuralgia (TN). That pain has a good prognosis. Sometimes it happens the other way around: Pain that resembles trigeminal neuralgia can be a warning sign of a possible stroke in the brainstem (medulla or medulla oblongata).
- In rare cases, a tumor is the cause of trigeminal pain.
- Inflammation of the nerve can also cause trigeminal neuralgia.
- IHA facial pain, or idiopathic trigeminal neuralgia, is a form of facial pain where the cause is unclear.
- Problems due to leaking fillings of a tooth or damage after tooth extraction.
- Too much nail biting, teeth grinding, lip biting or chewing gum can lead to overloaded chewing muscles.
- Inflammation in one of the sinuses.
Location of the trigeminal nerve
The trigeminal nerve, also called the fifth cranial nerve, runs from the brain stem to the face. You can find more information about this via this link.
Characteristics of the pain
Facial pain is a type of pain in the face that comes back in attacks. It involves short, intense "lightning bolt" pain attacks on one side of the face, in the area of an important nerve (the fifth cranial nerve (nervus trigeminus / trigeminal nerve).
This pain, like cluster headaches, is rated with the highest pain score: a 10 on a scale of 0 to 10.
The attacks begin and end abruptly, with a short duration of only 1 second to a maximum of 2 minutes.
Does a person feel the pain in the forehead? Then it is the first nerve branch.
Is the pain in the upper jaw, nostril or upper lip? That is the second branch.
Does a person have pain in your lower jaw, lower lip or tongue? Then it is the third branch.
The pain often occurs by touching a specific spot (trigger point) in the area; the nostril or the side of the tongue. Cold can also sometimes trigger the pain. Or making movements with the face, such as talking, chewing and swallowing.
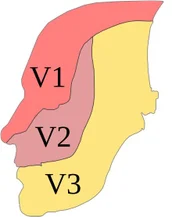
1. Pain in this area: V1 shows the first branch of the fifth cranial nerve trigeminal nerve
2. Pain in this area: V2 shows the second branch of the fifth cranial nerve trigeminal nerve
3. Pain in this area: V3 shows the third branch of the fifth cranial nerve trigeminal nerve
Between the pain attacks, a person usually has no pain and everything feels normal. There are also people whose face can feel a bit numb.
Tension headache
The term tension headache is misleading. Neither tension nor muscle tension is always the cause.
- A pressing, pinching pain as if there was a band around the head or on either side of the head
- Mild to moderate headache, less severe than migraine
- Often sensitive neck, shoulders and skull but rarely increased muscle tension in neck and shoulders,
- Sometimes light and sound sensitivity, but that is not standard with tension headaches
- Sometimes reluctance to eat
- Activities can still be carried out
- Tension is not necessarily the cause of this pain, but it can worsen with tension or incorrect posture
- Lasting minutes to days; episodic form (less than 15 days per month) and a chronic form (more than 15 days per month)
Cervicogenic headache
Pain from the neck
- Nagging, non-throbbing headache, sometimes in attacks
- Moderate to severe headache
- Headache complaints from the neck or back of the head, sometimes radiating to the frontotemporal area (side of the forehead) and above the eye
- On one side of the head, sometimes both sides
- Neck movement or positioning can make the pain worse
- Lasting hours to days
- Sensory overstimulation can, among other things, lead to temporary changes in the control of muscle groups from the cranial nerves
- This can cause muscle cramps and pain
Supra-orbital neuralgia
Nerve pain caused by damage to the supraorbital nerve
- One-sided headache of the forehead and eye
- Tingling, pricking, burning pain
- Pain may worsen when touched
- A test block of the nerve causing this pain can confirm the diagnosis
Withdrawal headache / Rebound headache
Sometimes medications taken for headaches or other pain can cause rebound headaches.
When pain medications are taken daily on a regular schedule, it can cause headaches if one or two doses are missed.
A 'rebound' headache can also develop if a person reduces the amount of daily caffeine such as in coffee, tea or energy drinks.
- Chronic headache
- Pressing pain
- Lasts all day
- Worse in the morning and with exertion
Migraine
Attack-like headache mild to severe. It varies per attack.
Migraine has different phases. These phases may overlap.
- The prodrome phase: 24-48 hours prior to an attack, one may experience complaints of:
- Fatigue
- Be less able to think well
- A change in mood. More sensitive, happier, more irritated, etc.
- Muscle stiffness in the neck
- Stomach and intestines (gastrointestinal complaints)
- Feeling like eating certain things
- More sensitive to light and sound
- Fatigue
- The aura phase: This phase occurs in 1 in 4 people. It usually comes on gradually over about 5 minutes, lasts about 1 hour and then disappears. Aura refers to temporary changes in sensory experiences (seeing, smelling, feeling) or temporary speech and language symptoms. Complaints that may occur:
- Seeing nothing on one side (hemianopsia)
- Sensory hallucinations
- Flickering patterns (flicker scotomas), seeing spots that slowly grow larger, change, become a sawtooth shape or move towards the outside of the eye
- Blurred vision, double vision, seeing waves or bright lines, seeing light
- Temporary hearing loss or tinnitus
- Dizziness
- Inability to feel or move a part of the body (for example, numbness in the tongue or on one side of the body)
- Tingling, numbness or burning pain in the face (for example the lips), hands or feet
- Less strength in one side of the body
- Seeing nothing on one side (hemianopsia)
- The postdrome phase: In this final phase, which lasts about 1 to 2 days, a feeling of exhaustion or a hangover predominates. Although some people feel exuberantly happy or very pleasant. Cognitive tasks, such as thinking and understanding, can be somewhat more difficult.
- There are people who have migraines without a headache. This is sometimes called a 'silent migraine', in which aura symptoms occur without a headache. This can vary from a few minutes to an hour.
- Hereditary factors, hormonal factors such as menstruation and external factors play a role.
- Migraine in itself is a brain disorder (neurovascular disorder).
- Studies show that migraines may be a risk factor for structural changes in the brain.
In 2012, research published in the Journal of the American Medical Association (JAMA) showed that very small abnormalities similar to cerebral infarctions were found in just under 10% of migraine patients.
In the cerebellum of the posterior bloodstream area come small
Infarctions are more common in migraine patients than in a healthy population.
Abnormalities in the white matter (white matter abnormalities WMAs), infarct-like lesions (ILLs), changes in gray and white matter (GM, WM) and cognitive damage were also found.
It was striking that white matter damage did occur in women (without aura during migraine) and not in men.
Brain infarctions due to migraine with aura also occur.
Other research showed small brain changes; decrease in gray matter, mainly in the visual cortex areas (V3 and V5), compared to control groups.
See for more information here.
Cluster headache
It is not known whether this headache can be triggered by brain damage, but we cannot rule out this cause.
- Strictly one-sided most severe headache
- Intense piercing stabbing flaming pain around and behind the eye,
- Sometimes accompanied by a watery eye or drooping eyelid, runny nose or red eye. This does not happen to everyone.
- Being unable to sit still due to pain does not happen to everyone
- Attacks lasting from 15 minutes to hours
- Cluster attacks can last several weeks to months, with the attack frequency varying from one every two days to eight per day/night. After such a period, the patient can be attack-free for months to several years.
- Rarer is the chronic cluster headache form (approximately 15% of people with this headache) in which there are no attack-free periods. This most serious form of headache can affect your entire life.
See for more information here.
SUNCT headache
SUNCT has been recognized and described since 2014. It is the abbreviation for ‘Short Lasting Unilateral Neuralgiform Headache Attacks with Conjunctival Injection and Tearing’.
SUNCT has attacks that are shorter than cluster headaches, but it also causes an intense, pulsating pain on one side of the head. This is accompanied by red, watery eyes and specific symptoms in the eye, such as a swollen eyelid. A person may blush and have a blocked nose during the attacks. The attacks last from a few seconds to ten minutes.
The cause of SUNCT is not yet fully known, but it is associated with disorders in the brain stem or nerve irritations.
The attacks resemble those of cluster headaches, as described above, but differ mainly in the duration of the attacks and the frequency. With cluster headaches, a person does not necessarily suffer from watery eyes.
advertisements are not ours
Resources
Al-Khazali HM, Ashina H, Iljazi A, Lipton RB, Ashina M, Ashina S, Schytz HW. Neck pain and headache after whiplash injury: a systematic review and meta-analysis. Pain. 2020 May;161(5):880-888. doi:10.1097/j.pain.0000000000001805. PMID: 31977938.https://pubmed.ncbi.nlm.nih.gov/31977938/
Arboix A, Massons J, Oliveres M, Arribas MP, Titus F: Headache in acute cerebrovascular disease: a prospective clinical study in 240 patients. Cephalalgia 1994;14:37-40.https://pubmed.ncbi.nlm.nih.gov/8200024/
American Migraine Foundation The Timeline of a Migraine Attack. https://americanmigrainefoundation.org/resource-library/timeline-migraine-attack/Cutrer FM. Pathophysiology, clinical manifestations, and diagnosis of migraine in adults. UpToDate. Available at https://www.uptodate.com/contents/pathophysiology-clinical-manifestations-and-diagnosis-of-migraine-in-adults. Accessed 8/24/2020.Hansen AP, Marcussen NS, Klit H, Andersen G, Finnerup NB, Jensen TS: Pain following stroke: a prospective study. Eur J Pain 2012;16:1128-1136. https://pubmed.ncbi.nlm.nih.gov/22407963/
Hoge CW, McGurk D, Thomas JL, Cox, AL, Engel CC, Castro C A (2008). Mild traumatic brain injury in u.S. Soldiers returning from iraq. N Engl J Med, 358(5), 453-463.Lahz S, Bryant RA (1996). Incidence of chronic pain following traumatic brain injury. Arch Phys Med Rehabil, 77(9), 889-891.Lew HL, Lin PH, Fuh JL, Wang SJ, Clark DJ, Walker WC (2006). Characteristics and treatment of headache after traumatic brain injury: A focused review. Am J Phys Med Rehabil, 85(7), 619-627.Marcus DA (2003). Disability and chronic posttraumatic headache. Headache, 43(2), 117-121.Mihalik JP, Stump JE, Collins MW, Lovell MR, Field M, Maroon JC (2005). Posttraumatic migraine characteristics in athletes following sports-related concussion. J Neurosurg, 102(5), 850-855.Kathleen R. Bell, MD, Jeanne Hoffman, PhD, and Thomas Watanabe, MD http://www.pmrjournal.org/article/S1934-1482(14)00308-6/abstract
O'Donnell MJ, Diener HC, Sacco RL, Panju AA, Vinisko R, Yusuf S: Chronic pain syndromes after ischemic stroke: PRoFESS trial. Stroke 2013;44:1238-1243. Pubmed/Medline (NLM)Seroussi R, Singh V, Fry A. Chronic whiplash pain. Phys Med Rehabil Clin N Am. 2015 May;26(2):359-73. doi: 10.1016/j.pmr.2015.01.003. Epub 2015 Mar 7. PMID: 25952070.https://pubmed.ncbi.nlm.nih.gov/25952070/
Sommerfeld DK, Welmer AK: Pain following stroke, initially and at 3 and 18 months after stroke, and its association with other disabilities. Eur J Neurol 2012;19:1325-1330. Pubmed/Medline (NLM)Weissenstein A, Luchter E, Bittmann MA. Alice in Wonderland syndrome: A rare neurological manifestation with microscopy in a 6-year-old child. J Pediatr Neurosci. 2014;9(3):303-304. doi:10.4103/1817-1745.147612.https://www.thuisarts.nl/hoofdpijn, http://www.pijn.com/nl/zorgverleners/pijndiagnose/pijndiagnoses-per-regio/aangezicht-hoofd-nek/cervicogene-hoofdpijn/https://www.ncbi.nlm.nih.gov/pubmed/9443481
https://www.ncbi.nlm.nih.gov/pubmed/23986301
Migraine and structural changes in the brain: a systematic review and meta-analysis Bashir A1, Lipton RB, Ashina S, Ashina M.
https://www.ncbi.nlm.nih.gov/pubmed/23986301 and https://www.ncbi.nlm.nih.gov/pubmed/24751961
https://www.ncbi.nlm.nih.gov/pubmed/14747499
Migraine as a risk factor for subclinical brain lesions.
https://www.karger.com/Article/FullText/375397#scrollNav-5
Onderzoek naar overprikkeling Hoe beïnvloedt overprikkeling het leven van mensen met Niet Aangeboren Hersenletsel. https://www.overprikkeling.com/onderzoek-overprikkeling
https://americanmigrainefoundation.org/resource-library/acute-migraine-treating-early