Rest in your nervous system
The nervous system is divided into several "systems" see image:
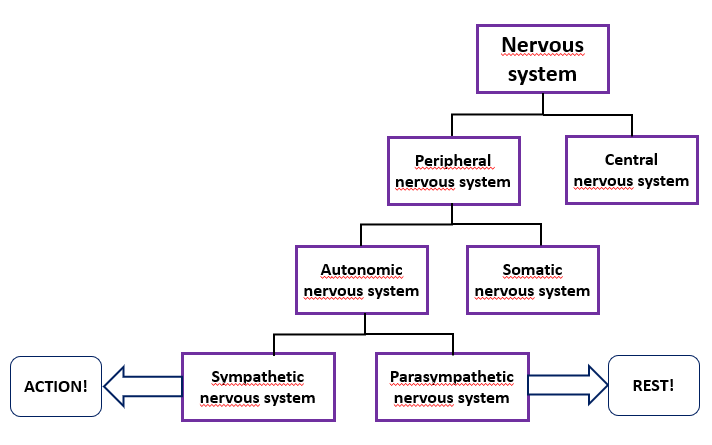
On this page we discuss two specific parts of the nervous system: the action part and the rest part.
- ACTION! The sympathetic nervous system: The nervous system that ensures that you can take action. That you can make an effort. This nervous system is also active during stress.
- REST! The parasympathetic nervous system: The nervous system that ensures relaxation and recovery of the body.
Brake and accelerator pedal of the body
You can think of these two nervous system systems as the brake and accelerator of the body.
The two systems are part of the autonomic nervous system. This means that everything happens automatically, without you having to think about it.
For example, breathing, blood pressure, digestion and so on.
Fortunately, we can exert influence somewhere in that automatically functioning nervous system to get the body into rest and recovery mode. The influence is limited and cannot heal the body, but it can promote rest and recovery from the day.
The parasympathetic nervous system can be activated through breathing. This way, an overactive or even cognitively overstimulated brain (due to many thinking tasks and thinking stress) can recover from the day or the action.
It is important to learn the difference between chest and abdominal breathing.
Chest breathing is intended to quickly supply oxygen to the body during action, but if a person continues to use chest breathing while resting, i.e. breathes 'high', the body remains in the action and stress mode.
Abdominal breathing gives the body rest.
Place both hands on the abdomen and feel the abdomen rise instead of the chest.
Breathing calmly, in through the nose, and making long exhalations puts the body in the rest and recovery position.
The calmer you breathe (abdominal breathing), the calmer the body becomes.
Normally the sympathetic and parasympathetic nervous systems are in balance, but people with brain damage experience much more stress in their lives due to the visible and invisible limitations
that they have to deal with.
They live, so to speek, permanently in "fight or flight, action! mode" with a depressed accelerator pedal, resulting in increased energy consumption due to increased heart rate, high blood pressure, delayed digestion, stress, tense shoulders and neck.
With constant stress, the body continuously produces stress hormones, which can also change the nervous system. This can also lead to complaints such as stomach problems, autoimmune changes, cardiovascular disease, muscle function changes, sleep disturbance and sleep problems, depression, burnout or anxiety disorders.
There are many brain injury victims who are in a continuous state of exhaustion due to chronic overstimulation*. [source surveys brain injury explanation]
At the moment of exhaustion, the body enters a vicious circle: imbalance produces imbalance.
Learning calm abdominal breathing, in addition to all other measures to bring peace and regularity into the life of someone with a brain injury, can provide a little bit of relief.
A small side note! People with brainstem injuries may have more difficulty breathing consciously. The respiratory center may be disrupted.
Specific information about burnout
People with a burnout appear to have a higher breathing frequency than an average person, as scientific research has proven. According to Erik Matser, clinical psychologist in Helmond, persistent stress affects the brain, causing it to function worse and the brain tissue can change.
Bart Oosterholt and Erik Matser conducted research at Radboud University Nijmegen in 2016 into the long-term cognitive effects of people with burnout (see source).
This study indicated that the cognitive impairments (such as working memory and reaction speed) of burnout can be long-lasting.
It is important to listen carefully to the first signs of burnout and act accordingly. Characteristic include prolonged fatigue and irritability.

Resources
Hersenletsel-uitleg, team neurologie
Jerath R, Crawford MW, Barnes VA, Harden K. Appl Psychophysiol Biofeedback. 2015 Jun;40(2):107-15. doi: 10.1007/s10484-015-9279-8. PMID: 25869930 Self-regulation of breathing as a primary treatment for anxiety.
Jonsdottir, I.H. , Nordlund, A., Ellbin, S., Ljung, T., Glise, K., Währborg, P., Wallin, A., (2013) Cognitive impairment in patients with stress-related exhaustion. 2013 Mar;16(2):181-90. doi: 10.3109/10253890.2012.708950. Epub 2012 Sep 17. https://pubmed.ncbi.nlm.nih.gov/22746338/
Mourya M, Mahajan AS, Singh NP, Jain AK. Effect of slow- and fast-breathing exercises on autonomic functions in patients with essential hypertension. J Altern Complement Med. 2009; Jul;15(7):711-7
Lehrer PM., Gevirtz R. Heart rate variability biofeedback: how and why does it work? Frontiers in Psychology. (5):2014; 756.
Oosterholt, B. G., Maes, J. H. R., Van der Linden, D., Verbraak, M. J. P. M., & Kompier, M. A. J. (2016). Getting better, but not well: A 1.5 year follow-up of cognitive performance and cortisol levels in clinical and non-clinical burnout. Biological Psychology, 117, 89-99. https://core.ac.uk/download/pdf/79163738.pdf#page=82
Weber, A,. & Jaekel-Reinhard, (2000) Burnout syndrome: a disease of modern societies? Institute and Outpatient Clinic for Occupational, Social and Environmental Medicine of the University of Erlangen-Nuremberg, Germany https://www.researchgate.net/publication/12131853_Burnout_Syndrome_A_Disease_of_Modern_Societies