Neurological Examination
Table of contents:
Introduction
General neurological examination:
1. Higher cortical functions, cognition, mood
2. Neck and neck area
3. Cranial (brain) nerves
4. Motor skills
5. Sensitivity
6. Reflexes
7. Coordination
8. Gait, stance and balance
9. Mnemonics for the doctor / including drainage area of blood vessels
Introduction
Most people with brain injuries have been assessed by a neurologist. Most will remember the little tests such as sticking out the tongue and bringing the finger to the nose or trying to walk in a straight line.
What most people do not know is that during a basic neurological examination, brain areas and the various nerve pathways, muscles, reflexes and coordination are systematically checked using these types of questions and tests. This allows the doctor to quickly assess where the injury is located. More specific injuries in:
- brainstem
- cerebellum / little brain
- subcortical injury (subarachnoid space - between cobweb and soft meninges - thalamus, basal ganglia, white matter - extensions of nerve cells in the brain, etc.)
- cerebral cortex (gray matter (brain cells) of the frontal lobe, temporal lobe, parietal lobe, occipital lobe)
The doctor also assesses the muscle reflexes, muscle strength, muscle tone (resting tension for the muscles), senses, gait (motor skills), coordination, sensory disorders, balance and checks each cranial nerve.
The doctor also asks questions to assess thinking and memory, thereby checking higher cerebral functions (mood, speech and language, orientation).
General neurological examination
1. Higher cortical functions
(cortex = cerebral cortex, cortical refers to the cerebral cortex)
Testing attention, orientation, memory, language, executive functions, praxis and visuo-spatial insight.
- Is the patient alert and conscious, how is the memory fuction and are there speech or language disorders?
- Does the patient know how to orient her- or himself in place, person and space? Does the he or she know what day and month it is? What are the starting points for recognizing cognitive problems during the conversation? Can the patient tell a coherent story of what happened? Can the patient remember a series of numbers for a short period of time and, for example, count backwards from 100 or count back in steps of seven from one hundred to a lower number?
The brain stem is always involved in a loss of consciousness. Furthermore, these three brainstem functions are always examined:
- Pupil reflex: Shine a light alternately into the right eye and the left eye. If there is an abnormality on one optic nerve, there will be no abnormality on either side a pupillary reflex occurs when the doctor shines into the affected eye. Conversely, if the doctor shines in the good eye, a pupillary reflex will occur in both eyes. If there is a difference in response between the two pupils or no pupil response, there is a problem in the brain. A disturbed pupillary reflex can show something about possible damage to the brain stem.
- Corneal reflex: The eyes will involuntarily close when the doctor touches the cornea. The absence of the corneal reflex is one of the tests required to diagnose brain death.
- Compensatory movements: The eyes continue to look at you when you move the head.
- Is there spontaneous speech, understanding of language? Can someone repeat, write and read a sentence?
- Is the pace of thinking slow?
Is there depression, anxiety or behavioral problem?
2. Neck and neck area
The position of the head is taken into account. If the patient has irritation in the meninges, she or he holds the head in excessive extension (hyperextension).
Is there neck trauma or osteoarthritis? If there is no trauma, can the chin be brought to the chest?
Brudzinski's sign: The patient's head is flexed quite abruptly. In case of meningeal irritation, a spontaneous bending of both knees occurs.
Kernig's sign: The hip is brought into a 90° flexion position and then the knee is extended. If there is an increase in pain in the neck when the knee is extended, there is definitely something wrong. The other leg is also tested. The suspicion of meningitis is thus confirmed.
3. The twelve cranial nerves
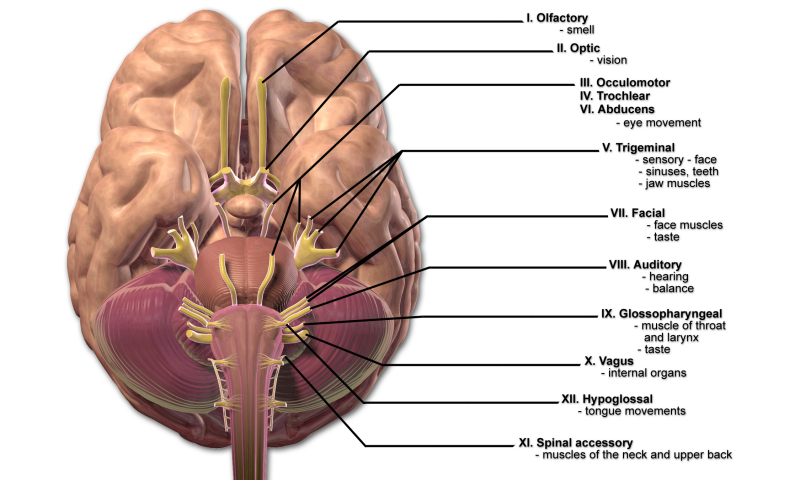
BruceBlaus. When using this image in external sources it can be cited as: Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010.
The patient is observed on the following aspects.
Is there a drooping eyelid (ptosis)? What is the pupillary reaction like?
Are there any deviations in the eye position? Eyeball motor skills: smooth eye tracking movements when the head is stationary?
No double vision (diplopia), no wiggling eyes (nystagmus), sense of feeling (sensitivity) of the face intact, no loss of vision? Is there a drooping corner of the mouth or an asymmetrical face? Does the patient have a hoarse voice, a nasal voice or does the person not speak fluently? That is, is there dysarthria?
In acute injuries, the cranial nerves can provide many clues:
- Papilledema (a swelling of the blind spot in the eyes) and cranial nerve IV weakness are associated with increased brain pressure (ICP).
- Involvement of cranial nerves III, V, and VI indicates a cavernous nerve sinus thrombosis.
- Cranial nerve involvement IX, X, XI and XII is an indication of Vernet syndrome when the jugular vein is affected by a clot (thrombosis), but it can also indicate a tumor, trauma or infection.
The 12 cranial nerves are systematically checked.
- Cranial nerve I, Nervus Olfactorius, the nasal function (smell) is tested with fragrances.
- Cranial nerve II, Nervus Opticus, the optic nerve or facial nerve. Each eye is tested separately.
- Visual acuity at a distance of six meters to read letters of different sizes
- Visual fields, does the patient see less than half or a quarter?
- Pupillary reflex (in case not yet tested for cranial nerve I)
- Accommodation reflex, the patient is asked to fix her or his gaze on the index finger of the doctor who is pointing it
approximately one meter away, in the center of the face. The finger is slowly moved to the tip of the patient's nose. Attention is paid to the reaction of the pupils (constriction = miosis).
- Visual acuity at a distance of six meters to read letters of different sizes
- Cranial nerve III, Nervus Oculomotorius controls all eye movements except looking outward (abduction) and looking down inward (which is done by the trochlear nerve cranial nerve IV). It also controls the raising of the upper eyelid.
- Cranial nerve IV, Nervus Trochlearis controls the inward gaze and therefore examination of this optic nerve is often done together with the examination of cranial nerves I, II and III.
- Cranial nerve V, Nervus Trigeminus is the facial nerve. This nerve controls facial sensation and the movement of the chewing muscles.
- The sense of feeling is tested with a cotton swab.
- The masticatory muscles are examined by palpation.
- Cranial nerve VI, Nervus Abducens regulates outward vision and therefore examination of this optic nerve is often included in the examination of cranial nerves I, II and III.
- Cranial nerve VII, Nervus Facialis is the motor nerve of the facial muscles. Symmetry in the face is examined.
- raising eyebrows
- frown
- close eyes firmly
- puffing out cheeks
- showing teeth
- pouting lips
- the doctor asks about saliva and production of tears
- the doctor asks about the feeling on one side of the tongue and asks about taste
In case of half-sided paralysis due to a stroke CVA deviations will quickly become visible here. The nerve can also become wedged in by a bridge angle tumor.
- Cranial nerve VIII, Nervus Vestibulocochlearis regulates hearing (and plays a role in balance). The doctor will test the hearing by tapping next to the ear and rubbing the fingers next to the ear. The doctor can also do a whisper test.
- Rinne's test: the vibrating tuning fork is held against the pointed protrusion of the temporal bone (mastoid). The patient is asked to indicate when he or she no longer hears vibration. Then the doctor will hold the still vibrating tuning fork in front of the ear and ask if anything is heard. A middle ear infection can also be detected in this way.
- Weber's test: the vibrating voice shape is placed in the center of the patient's crown. Does the patient hear the tuning fork in the middle or more in the left or right ear?
- Swabach's test: the vibrating tuning fork test is compared with the doctor's own hearing.
- Rinne's test: the vibrating tuning fork is held against the pointed protrusion of the temporal bone (mastoid). The patient is asked to indicate when he or she no longer hears vibration. Then the doctor will hold the still vibrating tuning fork in front of the ear and ask if anything is heard. A middle ear infection can also be detected in this way.
- Cranial nerve IX, Nervus Glossopharyngealis is the ninth cranial or tongue-pharyngeal nerve. The examination of this nerve takes place at the same time as the examination of the 10th cranial nerve, the Nervus Vagus. The nerve supplies sensory nerves: oropharynx, Eustachian tube, middle ear, posterior third of the tongue, carotid sinus, carotid artery, and gustatory to the posterior third of the tongue. It also serves motor nerves of destylopharyngeus.
The destylopharyngeus is a muscle in the head that extends between the pharynx and the temporal styloid process. It extends downwards below the ear. This helps the tongue and larynx to move.
The doctor will want to look inside the mouth to examine the motor function of the throat and pharyngeal arch. The pharynx is the head of the esophagus; the upper part of the respiratory and digestive systems.
- Cranial nerve X, Nervus Vagus is examined simultaneously with the 9th cranial nerve. The 10th cranial nerve controls many things such as heart rate, blood pressure, fainting (vagal response) and the digestive system and the muscles in the neck and chest. Both nerves (9 and 10) control the palate, the esophageal head (pharynx) and the larynx (larynx), which together control swallowing, making sounds and articulating.
- The tongue is pressed slightly with a spatula and the palate is examined and the patient is asked to say AAA or EEE. In case the palate does not pull up symmetrically, this is an indication of damage to motor fibers on the other side.
- If it is not clear whether something is functioning properly, the spatula or a cotton swab is pressed against the soft palate for a moment. In case at this moment a non-symmetrical image appears again or if there is no response, the patient is asked whether he or she feels anything. This can be used to determine whether there is damage to the sensory fibers of the 9th cranial nerve.
- Cranial nerve XI, Nervus Accessorius controls a two-headed muscle in the neck area (musculus sternocleidomastoideus) en the upper part of the monk's hood muscle (musculus trapezius).
- The doctor will ask to move the head from left to right while applying counter pressure to the lower jaw. Meanwhile, the doctor touces the the neck muscle on the other side and observe whether a normal muscle can be seen in the neck.
- The doctor will ask for a shrug. The doctor can apply firm counter pressure to the monk's cap muscle to estimate its strength
muscles.
- Cranial nerve XII, Nervus Hypoglossus controls the motor function of the tongue. It's the sublingual nerve.
- The patient is asked to open the mouth wide. The doctor examines the position and shape of the tongue. The doctor checks whether there are any abnormalities or muscle cramps (fasciculations).
- The patient is asked to stick the tongue straight out. If the tongue deviates to the left or right, this is a reason for further investigation to determine whether there is half-sided paralysis.
- The patient is asked to press the tongue against the cheek and the doctor then feels the force by feeling the cheek with the fingers.
- The doctor will ask the patient to move the tongue quickly from left to right.
Summary of the functions of the twelve cranial nerves
4. Motor skills
First of all, the doctor will look and observe. He or she checks for muscle cramps (fasciculations) that may be associated with anterior horn damage. The doctor will check whether there is a decrease in muscle tissue (atrophy) and compares left with right and involuntary movements (tremors, choreoathetosis) and persistent contractions of muscles (dystonia). Sometimes coordination tests are done immediately.
The doctor will check the flexor muscle of the arm (biceps), extensor muscle of the arm (triceps), wrist, extensor muscles, fingers, hip/lumbar muscle (iliopsoas), thigh muscle (quadriceps), hamstrings, foot lifts.
The following functions are also checked:
- Paralysis (one-sided - hemiplegia or bilateral), drooping corner of the mouth or eyelids, foot drop
- Muscle twitches (myoclonia), muscle contractions, vibrations (tremors)
- Decreased or rapid movements (chorea)
- Muscle loss (atrophy).
- Painfull muscles
- Muscle tone (the resistance generated by the passive movement of the limbs). In case of injury within the pyramid (areas that run from the cerebral cortex and the medulla oblongata to the spinal cord), the muscle tone (resistance of the muscle) is greatly increased. This also occurs after a cerebral infarction, for example. In Parkinson's there is also an increased muscle tone and also the cogwheel phenomenon. When the arm is moved passively, so-called cogwheel shocks are felt in Parkinson's.
- Muscle strength
- Neck stiffness check (including to detect meningeal irritation) People keep their neck in hyperextension when there is severe meningeal irritation
- Bend one hip and knee (to detect meningeal irritation)
- Barré's test: stretch arms in front of you for 30 seconds with eyes closed and fingers extended, affected side drops in case of pyramidal tract injury
- Mingazzini's test: legs in the air for 30 seconds, eyes must remain closed to prevent visual guidance. Examines motor skills of the lower limbs: dropping down of a leg or inability to keep the legs in place
- Combined test Barré-Mingazzini: in a lying position (on the back or on the stomach), keep the legs high with knees at 90°
- Gordon-Holmes test: While lying down, stretch the arms forward with eyes closed and palms facing up: different diseases, three different results depending on whether the arm drops or the hand turns inward or the arm does not return in original position
- Knee-heel test: Place the foot on the knee of the other leg. Examines coordination of the lower extremities. See also at 7 (coordination). In case of injury to the cerebellum, movements are jerky/ataxia. Multiple Sclerosis can also be tested with this.
- Walking on tiptoes: See 8. Gait, stance and balance.
- Walking on heels: See 8. Gait, stance and balance.
- Trendelenburg test (standing on one leg): there is a deviation when the pelvis (sometimes the whole upper body) sinks crookedly to the side of the leg on which one stands (affected side). Can also be observed when the patient walks. It may or may not show muscle weakness of the muscles that can move the leg outwards into the hip (hip abductors).
- Pinch force (squeeze the doctor's fingers)
5. Sensitivity
Sensitivity is divided into two parts:
- The vital sensitivity. Vital sensitivity is vital (vital). This involves the ability to feel hot and cold (temperature) and pain.
- The Gnostic sensitivity. This has to do with recognition. Gnostic sensitivity consists of the fine sense of touch, pressure perception, vibration sense, movement sense and position sense (proprioception). This concerns information that is created by movement, for example of the skin over an object.
Feeling (sensitivity) of the upper and lower limbs is checked to see whether there is loss or whether it is intact. The doctor checks symmetrical areas on the left and right, hands, feet, face and where complaints are reported. For example, a polyneuropathy or single nerve loss can be discovered or injury originating from the brain.
The patient must undergo the tests with his eyes closed.
- Pain sense: Does the patient feel pain when he or she touches the body with an object. The question is whether it feels blunt or sharp and whether it feels the same on the left or right.
- Sensitivity sense: Is something perceived when the limbs are stroked with a cotton ball. Is that the same on the left as on the right?
- Vibration sense: Is something perceived when a vibrating tuning fork is held against the limbs. In people over 60 years of age, the vibration sense is often reduced without there being any disease.
- Romberg's test: Does the person stagger or fall when the feet are together, the arms are extended forward and the eyes are closed? Or does the person remain standing?
- Temperature sense: Is a cold or warm object felt?
Reflexes
Basic rules when testing reflexes are:
- the patient must be relaxed,
- the arm or leg must be held at the correct angle
- the doctor must be able to use the reflex hammer with sufficient flexibility and force in a pendulum movement.
Injuries in the spinal cord are examined systematically. The reflexes in children are different than in adults.
Biceps tendon reflex: Test for the cervical vertebrae C5 and C6 by testing the upper arm muscle on the front of the arm for reflexes. The patient lies with the upper arm resting on the examination table and the forearm resting relaxed on the abdomen. The doctor places his own finger or thumb on the biceps and taps the upper arm muscle (biceps) with the reflex hammer. A contraction is felt in the biceps muscle.
Triceps tendon reflex: Test for the cervical vertebrae C3, C4, C5 by testing the upper arm muscle at the back of the arm. The patient lies while the elbow is pulled to a 90° angle. This triceps muscle is tapped with the reflex hammer and the forearm will stretch.
Knee-tendon reflex: Test for the lumbar vertebrae L2, L3, L4. The test can be done either lying down or sitting down. Sitting with hanging legs. The quadriceps muscle is tapped below the kneecap. MS can also be detected this way, among other things.
Achilles tendon reflex: Test for the sacral vertebrae S1 and S2. The patient's foot is placed at 90° to the lower leg while the physician supports the foot. The Achilles tendon is tapped. A bending will occur under the foot (plantar flexion).
Abdominal skin reflex: Test for the thoracic vertebrae T8, T9, T10 if tested above the navel and below the navel for the thoracic vertebrae T10, T11, T12. The abdomen should lie relaxed and a cotton swab or reflex hammer is stroked from the side of the abdomen (lateral) to the center of the abdomen (medial). Normally the navel pulls towards the performance of this test. If there is an asymmetry, it is abnormal.
Plantar reflex: the foot should not be pulled away. The back end of the reflex hammer is stroked across the sole of the foot from the heel. Normal reflex is to bend the big toe. Extension of the big toe (Babinski's sign) is abnormal and there is injury in the pyramidal tract.
Proprioceptive reflexes: twitch reflex/tendon reflex
7. Coordination
Top-nose test, top-top test, diadochokinesis, knee-heel test
Arms:
- Diadochokinesis: Make rotating alternating movements with both fingers raised; abnormally in case of injury to the cerebellum or alternately hitting the thighs with the palms and the back of the hand. The inability to perform opposing movements (disdiachokinesis or adiadochokinesis) occurs with cerebellar injury, upper motor neuron injury, and extrapyramidal disorders.
'Extrapyramidal' concerns all parts of the brain outside the pyramidal tract; Commands are given from the motor cerebral cortex to activate muscles, which carry out a planned movement.
- Top-nose test / finger-nose test: Finger in a large arc to nose. Alternate left and right fingers while eyes are closed.
This distinguishes deep sensory disorder from cerebellar/cerebellar problems/ataxia. It examines the coordination of the upper
limbs and whether the movement misses its target. This test is often abnormal in case of MS.
- Top-tip test: finger to examiner's fingertip
Legs:
- Knee-heel test; Place the heel on the knee and then slide the knee down over the shin, at first with eyes closed and then with eyes open. This requires muscle strength.
In case of injury in the cerebellum, the movements are jerky. This indicates ataxia.
Multiple sclerosis can also be tested with this. See also 4. Motor skills
8. Gait, stance and balance
Coordination is also tested in these tests.
- Gait: Patient has to take a considerable number of steps. Is there a wide aisle? This could indicate coordination difficulties in the cerebellum. What is the stride length? Does the patient move his arms?
- Heel and toe walking: if the patient has problems walking on his or her heels, this could indicate damage to the lumbar spine, of the fifth vertebra (L5). If the patient has difficulty walking on his or her toes, this could indicate damage to the sacral spine, the first vertebra (S1). Loss of muscle strength only becomes apparent after a few meters.
- Tightrope Walking: This is the test in which the patient has to walk in one line, one foot at a time. The heel is placed against the toe.
At first, the patient is allowed to look at his feet during the test.
After that, the patient should look straight ahead. After that, the eyes should be closed.
Standing and balance are assessed with the following tests:
- Rising from a squat: The patient attempts to rise from a squat while the doctor holds the patient's hands. This examines muscle weakness in the muscles closer to the trunk (proximal).
- Unipodal position: This is the test in which the patient has to stand on one leg while raising the knee of the other leg. After this, the patient has to stand on the other leg.
- Romberg's test: The patient is asked to connect the feet to eachother and lift the arms horizontally forward. The doctor is ready to catch the patient to prevent falling. Balance is first assessed with the eyes open and then with the eyes closed. There may be a proprioceptive disorder if the patient becomes noticeably unbalanced when the eyes are closed.
Mnemonics
The doctor will focus on the main complaint of the consultation and will try to quickly rule out things.
There are several usable mnemonics.
ABC
Airway, Breathing and Circulation Are the airways clear, is there breathing and blood circulation, is the heart working?
The 4 A's
Does the patient show signs of cortical (cerebral cortex) injury?
Aphasia: assesses comprehension, naming, repetition.
Apraxia: pretend to brush your teeth, light a match, use scissors
Agnosia: the need to recognize a small object in the hand with the eyes closed.
Anopsia: controls the quadrants in the visual field.
The 4 D's
Does the patient have signs of injury in the brainstem or cerebellum?
Diplopia: (double vision) check of the extraocular muscles / eye movements upwards, downwards to the side, looking inwards / strabismus, double vision.
Dysarthria: assesses fluency. The content is normal but the person has difficulty speaking and is less intelligible.
Dysphagia: Whether there is a lump in the throat or difficulty swallowing.
Dysmetria: The finger-nose-finger testing, rapid alternating movement. With dysmetria, the movement misses its target. In ataxia the movement is jerky.
SOAP
Subjective complaints, Objectively, Analysis, Plan of approach, see also here
Failure symptoms consistent with disruption of the blood supply in the various river basins, see here
Emergency room
- Cerebral infections (egencephalitis, brain abscess) are usually accompanied by changes in consciousness and fever
- Metabolic encephalopathy (for example due to hyponatremia, hypoglycemia and/or hypercalcemia) may be accompanied by symptoms of loss. In general, however, the subacute onset of changes in consciousness is in the foreground
- Subdural hematoma is rarely accompanied by acute, sometimes transient, symptoms
- Subarachnoid hemorrhage is characterized by acute, very severe headache and possible loss of consciousness
Resources
B. Zonneveld, Het neurologisch onderzoek, Utrecht 1992. ISBN 90-6348-067-9
Neurologie, 7e druk, Bohn Stafleu van Loghum, ISBN 97 8903 681 1880 medewerking van dr. A. Hijdra, prof. dr. P. Koudstaal, prof.dr. R.A.C Roos, mei 2017
SOAP for neurology
https://docplayer.nl/14687801-Het-neurologisch-onderzoek.html
https://www.domusmedica.be/documentatie/downloads/studiedagen/praktische-vaardigheden-22-11-2014/1040-neurologisch-onderzoek-1/file.html
http://www.skillslab.ugent.be/PDF/SkillslabNeuro1112.pdf
Het teken van Hoffman- Trömner
https://www.hopkinsmedicine.org/health/conditions-and-diseases/neurological-exam
https://my.clevelandclinic.org/health/diagnostics/22901-romberg-test