Encephalopathie
Literally translated, the word encephalopathy means brain disease. Enképhalos = brain, páthos = disease. Encephalopathy belongs to the diffuse brain injury types. This means that damage is not specific to one spot in the brain, but spread out all over the brain.
An EEG, an electroencephalogram (brain film of electrical activity), often shows a diffuse slowing in encephalopathy. That is, slow brain waves spread everywhere throughout the brain.
Encephalopathy is a general term without specifying the cause. The cause is often written before the word encephalopathy.
In alphabetical order
A
- Anoxic encephalopathy is the acute form of reduced brain function due to oxygen deprivation. This may be as a result of resuscitation, near-drowning, suffocation, cardiac arrhythmias, heart failure, status epilepticus (prolonged seizure of seizures), shock, accident. It can also occur in infants due to oxygen deficiency during pregnancy or at birth (perinatal asphyxia = oxygen deficiency around birth).
Other names are:
- Hypoxic ischemic encephalopathy (HIE)
- Asphyxia
Brain cells, kidney cells and liver cells are sensitive to oxygen deficiency. Of the brain areas, in particular the basal nuclei (basal ganglia) and in case of extensive oxygen deficiency, the cerebral cortex (especially the temporal lobe), hippocampus, brainstem and thalamus are very sensitive to oxygen deficiency. Damage to the basal nuclei can cause difficulty in movement, dystonia and spasticity. Damage in the cerebral cortex can cause difficulty moving, hearing, seeing and speaking. Brainstem damage can cause problems with all autonomic functions, such as temperature regulation, heart rate, blood pressure, breathing, sucking (in infants) and swallowing. Epilepsy can be a result of anoxic encephalopathy. Damage is not always visible on an MRI scan. Detectable abnormalities on an MRI scan can sometimes only be visible after a few days, but they can also disappear. Read more on our page on oxygen deficiency.
B
- Bovine spongiform encephalopathy (BSE or mad cow disease) Evidence for transmission of BSE to humans has not been provided, but there are significant similarities between BSE in cows and a new variant of Creutzfeldt-Jakob disease (CJD) in humans. This can be caused by eating beef from cattle infected with BSE. Read more here.
C
- Chronic Toxic Encephalopathy (CTE or Organic Psycho Syndrome OPS, also known as Painter's Disease) is one of the best-known forms of toxic encephalopathy. In case a person has regularly inhaled solvent fumes for years, symptoms of chronic intoxication with memory disturbances, difficulty concentrating, mental slowness, aggressive behavior, emotional lability, fatigue and depression may develop.
Read more here
- Chronic Traumatic Encephalopathy (CTE); progressive neurological deterioration of the brain due to much head trauma, as can occur in many types of sports. The accumulating effect of repeated head injuries with or without obvious symptoms such as a concussion and how long the exposure to the repeated head injuries took place (for example during the sports career) are determining factors. Read more on our page on CTE.
- COVID-19 Encephalopathy
Studies are underway into forms of encephalopathy that can be directly linked to COVID-19. We will post information on this site as soon as more information becomes available. Preliminary info can be found here.
Brief summary: Patients with COVID-19-associated encephalopathy present with symptoms such as dizziness, headache, anxiety and depression, stroke, seizures, Guillain-Barre syndrome (GBS) and demyelinating disease. The exact pathological basis for these neurological symptoms is currently unknown.
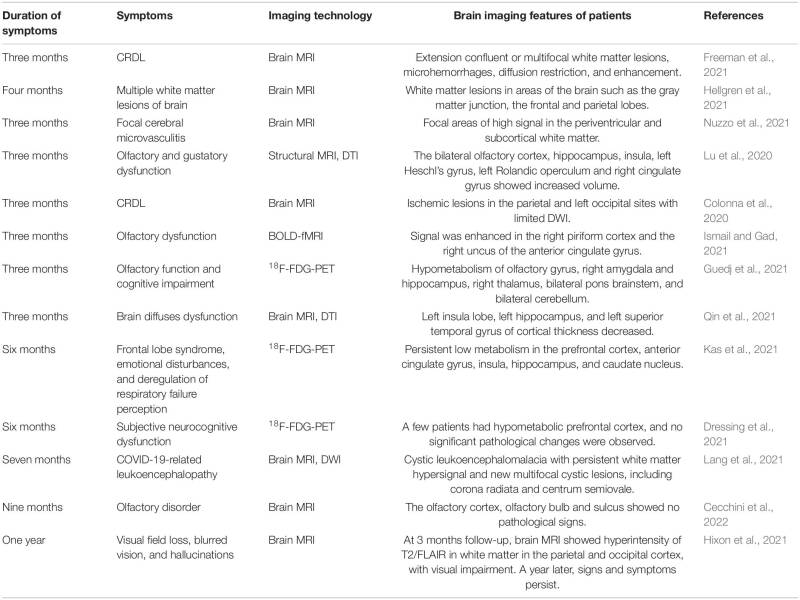
Studies have been done on changes in brain microstructure after 3 months, 6 months and 1 year after rehabilitation. See
image
H
- Hashimoto encephalopathy (SREAT); reduced brain functioning due to an immune or inflammatory response. Antibodies are produced in the blood against the thyroid gland, but also against the brain. The disease is seen in people with Hashimoto's disease
, an inflammation of the thyroid gland. This will cause the thyroid gland to work increasingly slowly. This slower functioning of the thyroid gland is called hypothyroidism.
Possible complaints:
- cognitive problems (difficulty concentrating, forgetfulness)
- behavioral changes
- confusion, disorientation
- disease image reminiscent of dementia
- psychiatric picture (psychosis, including visual hallucinations,
- hearing voices and paranoid delusions)
- aggression
- seizures
- difficulty speaking, walking, sleeping
- shaking hands (tremor)
- fever
- headache
- loss of visual field
- reduced consciousness
- coma
SREAT, the English abbreviation, means Steroid Responsive Encephalopathy Associated with Autoimmune Thyroiditis.
The disease can be treated with corticosteroids, such as Prednisone or Prednisolone.
The diagnosis can be made if there are no other causes for the brain not functioning properly, and if antibodies against the thyroid gland are found in the blood. The diagnosis is complete if the patient responds well to corticosteroid treatment.
- Hepatic Encephalopathy (HE) is a reduced functioning of the brain due to severe liver failure, for example due to liver cirrhosis. As a result, certain breakdown products can enter the blood circulation, such as ammonia, and the astrocyte brain cells 'swell'. Due to the swelling, the brain cells are less able to transmit signals. A sliding, sometimes not clearly noticeable deterioration in functioning can be seen, sometimes with periodic complaints (episodes). If someone shows a decreased level of consciousness without clear brain area related complaints (focal symptoms), a metabolic encephalopathy (due to accumulation of waste products) should always be kept in mind.
Possible complaints: reduced alertness, confusion, confused speech, dysarthria, word finding problems, change in fine motor skills and coordination, dizziness, daily activities are performed less well (apraxia), mood changes, sleep arrhythmias, sleepiness (hypersomnia) and insomnia, slowness, tremors (flapping tremor in which the fingers of the outstretched arm rise and fall sharply, also called asterixis or negative myoclonus; sudden loss of tone (muscle tone) of wrist and hand muscles and therefore an inability to maintain a fixed position of the hands), increasing disorientation , changed sense of time, fears, decreasing consciousness and finally hepatic coma. Other causes of an increase in ammonia include swallowing too many diuretics or benzodiazepines, valproic acid use (anti-epileptic drug), taking apparently harmless dietary supplements that can lead to liver damage and failure weeks to months after ingestion, infection, constipation and bleeding high in the gastrointestinal tract. A neurological examination and MRI scan do not have to show any abnormalities, diffuse brain damage can be detectable on an EEG. Abnormal laboratory values, such as elevated transaminase levels and elevated ammonia concentration, may not be present in every patient with HE.
- Hypertensive encephalopathy
Hypertensive encephalopathy is reduced or non-functioning of the brain as a result of severe high blood pressure. High blood pressure can cause the brain to receive insufficient blood supply to maintain functions. It is an emergency because the patient can quickly fall into a coma and die. However, it is a very rare condition. If properly treated with blood pressure-lowering medication through an IV, the symptoms can disappear and a person can recover.
Other causes of this hypertensive encephalopathy are acute kidney inflammation (nephritis), sudden discontinuation of medications for high blood pressure, renal artery thrombosis, Cushing's syndrome (disease with too much cortisol, a stress hormone in the body),
enpheochromocytoma (a tumor of the adrenal medulla that produces too much of the stress hormones adrenaline and norepinephrine). This condition can also occur in pregnant women who suffer from pre-eclampsia or eclampsia, but also in drug users; LSD (lysergic acid diethylamide), amphetamine and cocaine.
- Possible complaints:
- Sudden onset of severe headache
- dizziness
- confusion
- blurred or reduced vision
- nausea or vomiting
- epileptic attacks
L
- Lead encephalopathy due to lead poisoning
Toxic encephalopathy can also be caused by lead poisoning. Read more on this page of our website.
M
- Metabolic encephalopathy is a collective term for a reduced functioning of the brain due to an accumulation of waste products from the body, such as in uremic encephalopathy and hepatic encephalopathy. An EEG can show diffuse delay in metabolic encephalopathy; brainwaves with a frequency of 0–4 Hz, or delta waves.
- Minimal Hepatic Encephalopathy (MHE) is a lighter variant of hepatic encephalopathy, in which patients with cirrhosis of the liver function apparently well, but in which cognitive impairments can occur.
P
- Portal Systemic Encephalopathy is the milder variant of hepatic encephalopathy caused by chronic liver disease, usually due to liver cirrhosis, is often characterized by a more insidious development. Subtle cognitive dysfunction or periods (episodes) of "mild" neurological symptoms.
- Post anoxic encephalopathy is the chronic situation of impaired brain functioning due to oxygen deficiency, or local and temporary bloodlessness of a cerebral blood vessel. For a detailed description, see above under A: anoxic encephalopathy.
This situation can also occur after resuscitation in case of circulatory arrest (cardiac arrest and cessation of breathing), near-drowning, serious breathing disorders and severe low blood pressure, shock.
- Posterior reversible encephalopathy syndrome (PRES) / Reversible posterior leukoencephalopathy syndrome
Leukoencephalopathy means that the white matter of the brain is affected. White matter is the covering of nerve fibers. The brain therefore functions less well. Posterior means that it mainly concerns brain areas located at the back of the head.
Reversible means that complaints can disappear and can be cured. In most people, neurological disorders disappear within two weeks of treatment. Other names are acute hypertensive encephalopathy: rapidly occurring complaints due to less functioning brain caused by high blood pressure. Another name for the condition is 'reversible posterior leucoencephalopathy' (RPLE). - Symptoms may include:
- behavioral changes
- confusion
- agitation
- decreased consciousness
- nausea and/or vomiting
- headache
- cortical blindness and/or other visual complaints
- epileptic seizures, often starting with jerking of arms or legs
CT and MRI scans show extensive white matter abnormalities on both sides (bilateral) without visible infarction. This indicates edema (fluid retention) in the posterior areas of the cerebral hemispheres (occipital and sometimes parietal), or the brainstem or the cerebellum / little brain.
- Progressive multifocal vascular leukoencephalopathy (PML)
This is a rare form of a brain disease caused by a virus (JC virus / JCV, a human polyomavirus) that mainly affects people with reduced resistance. This virus normally causes mild symptoms of a cold, but remains present in the body and can flare up again when the immune system has decreased significantly.
The reduced resistance may, for example, be a result of immunosuppressive treatments. These are drug treatment of autoimmune diseases, such as rheumatism, multiple sclerosis or SLE. Medications given after a transplant for prevention also fall under immunosuppressive treatments. People with leukemia are also at risk of developing PML.
It can also be due to malignant blood diseases, sarcoidosis, or infection with HIV (almost 85% of cases).
Leukoencephalopathy means that the white matter in the brain is damaged. The white matter is the protective layer, myelin layer, around the nerve pathways. This becomes inflamed in PML. The result is disturbed stimulus conduction.
Multifocal means that there are abnormalities in multiple places in the brain. Progressive means that a disease progresses and new complaints quickly arise. It can lead to serious neurological and neuropsychological complaints such as:- changes in behavior
- cognitive disorders
- motor weakness (movements, muscle strength)
- difficulty walking and coordination disorders
- difficulty seeing
- difficulty with speech
- headache
- seizures
S
- Susac's syndrome
This rare disease is also called SICRET syndrome
(SICRET= small infarctions of cochlear, retinal and encephalic tissu) or Retinal cochleacerebral vasculopathy. This means that blood vessels in the brain, eyes (retina) and inner ear (cochlea) are inflamed and narrowed. Not all symptoms are obvious from the start, which can make it more difficult to reach a diagnosis. Sometimes it starts with eye complaints or with hearing complaints and sometimes with neurological complaints.The syndrome often shows the same symptoms as MS, but it is a completely different disease.
This syndrome is believed to be an autoimmune condition; an immune response against one's own body. This causes the small blood vessels to become inflamed and insufficient blood reaches the brain, eyes and ears. It is still unknown why only these small blood vessels are affected. More information about this syndrome on this website. The disease can affect the following organs:
Retina
If only the edge of the retina is affected, vision problems are less noticeable. Otherwise, parts of the visual field may disappear in one or both eyes. Complaints of blurred vision and light sensitivity (photophobia) are mentioned.
Inner ear
Hearing impairment/hearing loss may occur. Very specifically, the tip of the cochlea in the inner ear can become damaged, making low tones in particular less audible. If other areas of the cochlea are affected, someone may have problems with balance. Dizziness (vertigo) and ringing in the ears (tinnitus) are mentioned.
Brain
The complaints from the brain can include cognitive problems such as loss of concentration, memory problems and fatigue.
Behavioral changes such as confusion, disorientation, irritable or withdrawn behavior. Psychotic behavior can also occur. Severe headache throughout the head and migraine-like headache attacks. Sometimes epileptic seizures occur, but also myoclonia (muscle twitches) in the arms or legs. Sometimes a temporary loss of strength occurs. Muscle and/or joint pains are also mentioned.
Symptoms of failure may occur; change in strength or sensation, speech disorders, eye movement disorders and ataxia: balance and coordination problems.
Skin
Sometimes a marble-like pink-red discoloration is seen on the skin (livedo reticularis) or a red skin discoloration is visible on the trunk or feet.
T
- Toxic encephalopathy
Toxic encephalopathy is a neurological disorder caused by exposure to heavy metals such as lead, manganese, etc. or to neurotoxic organic solvents such as toluene.
Exposure to toxic substances can lead to a variety of neurological complaints. In addition to this toxic encephalopathy, symptoms similar to Parkinson's disease (parkinsonism) may occur.
and prevent nerve damage in several places in the body with sensory damage or pain (polyneuropathy).
A number of international criteria have been drawn up to diagnose 'toxic encephalopathy':
- prolonged and intensive exposure to organic solvents,
- complaints such as reduced concentration, memory disorders,
- fatigue, emotional lability, attention disorders, loss of initiative and depression (the complaints mentioned indicate a
organic psychosyndrome), - abnormalities in neuropsychological examination,
- a clear correlation in time between exposure and the development of the complaints.
U
- Uremic encephalopathy is a reduced functioning of the brain due to renal failure with an accumulation of breakdown substances, including serum calcium, which causes uremia to develop. It is the main complication of acute and chronic renal failure and requires urgent dialysis treatment. There is an imbalance in the neurotransmitter amino acids. Glycine levels rise and glutamine and gamma-aminobutyric acid (GABA) levels fall. Dopamine and serotonin levels also change. The symptoms vary from sensory disturbance, severe organic fatigue, seizures to coma, depending on the severity of the kidney failure.
V
- Viral encephalopathy is a reduced functioning of the brain due to a rare complication of the flu (influenza) and other viral infections. This also includes the corona virus. It is also called an acute necrotizing encephalopathy. Necrotizing means that brain cells die. See also viral encephalitis.
W
- Wernicke encephalopathy
Life-threatening vitamin B1 deficiency. People who are addicted to alcohol may have a vitamin B1 deficiency (thiamine deficiency). A potentially life-threatening complication of such a vitamin B1 deficiency is Wernicke encephalopathy.
A Wernicke encephalopathy can also be caused by: malnutrition or frequent vomiting (by whatever cause), which also prevents the absorption of vitamin B1 (thiamine).
Three symptoms (triad) are characteristic: confusion, coordination problems (ataxia) and paralysis of the eye muscle
(ophthalmoplegia).
Complaints of hearing loss are also mentioned but do not fall under 'the triad'.
If there are only two features of the Wernicke encephalopathy triad, plus a history of malnutrition, that is also a clue to the diagnosis.
Intravenously administered thiamine usually confirms the diagnosis
and in many cases causes the complaints of oculomotor abnormalities (vestibuloo-ocular reflex VOR)
, eye muscle weakness and auditory speech comprehension.
Vitamin B1 (thiamine) is not made in the body itself, but must be absorbed through food, such as grain products, potatoes, egg yolk, liver,
Before vitamin B1 has reached a critical lower limit, an acute and life-threatening condition develops: diabetes
Wernicke encephalopathy
or Wernicke's syndrome.
The complaints can progress to a coma and lead to death. However, this clinical picture is not always clearly present.
In this phase, Korsakov's syndrome can still be prevented by giving a large amount of vitamin B1 in the form of injections.
Sources
Amodio P, del Piccolo F, Marchetti P, Angeli P, Iemmolo R, Caregaro L, et al. Clinical features and survival of cirrhotic patients with subclinical cognitive alterations detected by the number connection test and computerized psychometric tests. Hepatology. 1999;29:1662-7.
Canan Akman, Dilek Ülker Çakır, Serkan Bakırdö˘,Serdal Balcı (May 2019). The Effect of Serum Calcium Levels on Uremic Encephalopathy in Patients with Acute Kidney Injury in the Emergency Department. Medicina (Kaunas, Lithuania) 55(5):204 · May 2019 DOI: 10.3390/medicina55050204
Fraser, C.L.; Arie, A.L. Nervous system complications in uremia. Ann. Intern. Med. 1988, 109, 143–153.
Hashimoto Encephalopathy: A Rare Intricate Syndrome –Payer, Petrovic, Lisy, Langer –(PubMed)
Lameire, N.; Van Biesen,W.; Vanholder, R. Acute renal failure. Lancet 2005, 365, 417–430.
Lizardi-Cervera J, Almeda P, Guevara L, Uribe M. Hepatic encephalopathy: a review. Ann Hepatol. 2003;2:122-30.
Lohr, James W., Batuman, Vecihi. (May 2017). Uremic Encephalopathy: Medscape
Mas A. Hepatic encephalopathy: from pathophysiology to treatment. Digestion. 2006;73 Suppl 1:86-93.
Häussinger D, Schliess F. Astrocyte swelling and protein tyrosine nitration in hepatic encephalopathy. Neurochem Int. 2005;47:64-70.
Häussinger D, Schliess F, Kircheis G. Pathogenesis of hepatic encephalopathy. J Gastroenterol Hepatol. 2002;17 Suppl 3:S256-9.
Smogorzewski, M.J. Central nervous dysfunction in uremia. Am. J. Kidney Dis. 2001, 38 (Suppl. 1), 122–128.
Steroid responsive encephalopathy associated with autoimmune thyroiditis (SREAT) or Hashimoto’s encephalopathy: a case and review; Lee SW at al.Vaquero J, Chung C, Blei AT. Brain edema in acute liver failure. A window to the pathogenesis of hepatic encephalopathy. Ann Hepatol. 2003;2:12-22.
Whitfield, C.L. (1972)
Lead encephalopathy in adults - ScienceDirect https://www.sciencedirect.com/
Vaquero J, Chung C, Blei AT. Brain edema in acute liver failure. A window to the pathogenesis of hepatic encephalopathy. Ann Hepatol. 2003;2:12-22.