Subdural hematoma
Summary
A subdural hematoma is a serious condition in which blood accumulates between the dura mater and the brain.
This may occur due to head trauma, such as a fall or accident, but it may also occur spontaneously in people with increased risk of bleeding and in elderly people.
The danger of a subdural hematoma lies primarily in the pressure it exerts on the brain. This can lead to symptoms such as headache, nausea, confusion, impaired coordination, loss of consciousness and, in severe cases, permanent brain damage or death.
Further explanation
A subdural hematoma, or subdural hemorrhage, occurs between the dura mater and the second membrane surrounding the brain, the arachnoid. Subdural means beneath the dura mater.
The bleeding is outside the actual brain tissue. However, the bleeding or hematoma may be life-threatening because it presses on the brain tissue and can cause injury.
It usually involves a ruptured artery.
The bleeding often results from an accident involving a contusion of the brain (cerebral contusion). It is then classified as a traumatic brain injury. Sometimes a subdural hematoma forms on the opposite side of the brain from where the impact occurred.
A subdural hematoma sometimes develops due to blood vessel problems, the use of blood thinners, or direct damage to the veins in the head (venous sinuses).
In children/adolescents, the cause may be an arachnoid cyst.
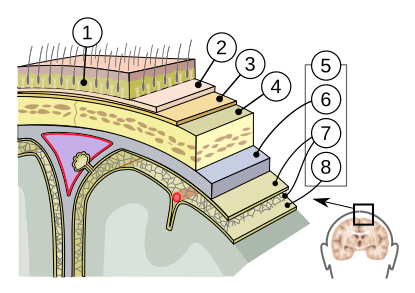
The Meninges
The meninges surround the brain. They nourish the brain and also serve as a cushion, protecting it.
The layers are constructed from the outside in:
- Scalp (1)
- Periosteum (2)
- Bone (3)
- Dural meninges (dura mater with two layers (4))
- Arachnoid mater (arachnoid (5))
- Subarachnoid space
- Pia mater (6)
1: skin
2: aponeurosis
3: periosteum
4: skull
5: meninges:
- 6: dura mater
- 7: arachnoid mater
- 8: pia mater
The dura mater
The dura mater lies directly against the skull. It consists of two layers:
- the periosteal layer, on the bone side. It forms a single unit with the periosteum of the skull
- the meningeal layer, on the brain side
There are blood vessels in a number of places between the two layers.
Three time periods for the formation of a subdural hematoma
A subdural hematoma may develop over three time periods:
- acute - the hematoma forms immediately after the initial injury
- subacute - the hematoma develops up to about a week after the initial injury (sometimes a little longer)
- chronic - the hematoma develops over a period of approximately two to three weeks after the injury.
These periods are not clearly defined.
Causes
Acute subdural hemorrhage usually occurs after a serious head injury, such as a car crash, physical assault, or a serious fall. This causes blood vessels to rupture. It is a medical emergency and surgical intervention is necessary. The prognosis is uncertain.
Chronic subdural hemorrhage usually occurs in older people. Brain tissue decreases with age, but may also be reduced by chronic alcohol use, which slightly widens the space between the skull and the dura mater.
The blood vessels are then more vulnerable to trauma, and there is a greater risk of bruising. This may cause a bleeding to become larger unnoticed and symptoms may appear later.
It is also possible that someone has an accident after which everything seemed fine. She or he could walkand talk and was clearly conscious. Days later, that person may be admitted to the emergency room with drowsiness, loss of strength, and headaches.
Brain scans may reveal a subdural hematoma and even a shift of the brain beyond the midline and ventricles. This is called a midline shift.
See our specific explanation on midline shift.
See image:

Image source: https://commons.wikimedia.org/w/index.php?curid=19364350
Even a minor accident, such as hitting your head against a window frame or a trunk, can cause a brain hemorrhage. Blood vessels may also burst due to frequent coughing or sneezing.
Many patients cannot recall an accident. The condition develops gradually and can include drowsiness, confusion, speech and cognitive disorders, and possibly half-sided paralysis. It resembles dementia. As the hemorrhage becomes larger, it puts more pressure on the brain, and a person may become more confused, experience seizures, and experience a loss of consciousness.
Vascular disorders may be another acute cause of a subdural hemorrhage.
For example: arteriosclerosis, high blood pressure, arterial aneurysms or arteriovenous malformations (AVMs).
Sometimes the cause lies precisely in anticoagulant medication used to treat these conditions.
This risk makes it difficult for a doctor to make the right decision about whether or not to prescribe blood-thinning medication. A subdural hemorrhage is an intracranial hemorrhage, a bleeding that occurs within the skull.
Symptoms
A subdural hematoma may be accompanied by one or more of the following symptoms:
- headache nausea (sometimes with vomiting) paralysis of an arm or leg
- speech problems
- seizures with jerking of the arms and legs
- mental decline (confusion, forgetfulness, behavioral changes)
- incontinence
- drowsiness and/or drowsiness
- loss of consciousness.
A subdural hematoma may be fatal in severe cases.
Treatment
Treatment depends on the severity of the bleeding and the symptoms.
In mild cases, rest and medical monitoring may be sufficient, allowing the body to gradually absorb the blood.
In more severe cases, surgery, such as a craniotomy or a drainage procedure, may be necessary to remove the blood and relieve pressure on the brain.
By drilling small holes in the skull, the hematoma can be drained.
If a thick capsule has formed, it has to be be removed through a small opening.
In cases of chronic hemorrhage, the skullcap usually heals only after several weeks, because the brain first needs to expand.
The condition sometimes affects both sides. The prognosis for a chronic subdural hematoma is good. Unfortunately, the prognosis for an acute subdural hematoma is poor.
The severity of the consequences also depends on whether the brain area was compressed for a short or a long period of time and whether the damage was temporary or permanent.
Drawing above: A hemorrhage and a bruise between the dura mater and the arachnoid mater
A video about a subdural hematoma:
Read more:
Clear images on subdural hematoma can be found here: https://radiologyassistant.nl/neuroradiology/hemorrhage/traumatic-intracranial-haemorrhage
Our website:
- Our page on stroke
- Our page on blood vessels of the brain
- Our pages on neurological, invisible and cognitive consequences
Other websites:
https://my.clevelandclinic.org/health/diseases/21183-subdural-hematoma
https://www.nhs.uk/conditions/subdural-haematoma/
https://emedicine.medscape.com/article/1137207-treatment
Resources
Subarachnoid haemorrhage. (2018, 10 december). van https://www.nhs.uk/conditions/subarachnoid-haemorrhage/
De Nederlandse Hartstichting. (z.d.). Oplossingen voor een sterk hart | Hartstichting. Consulted on 10th of may 2016, van https://www.hartstichting.nl/
Eyskens, E., Feenstra, L., Meinders, A. E., Vandenbroucke, J. P., & Van Weel, C. (1997). Codex Medicus (10e ed.). Maarssen, Nederland: ElsevierGezondheidszorg.
Hartwijzer. (z.d.). Consulted on 10th of januari 2016, van https://www.hartwijzer.nl/
Hersenletsel-uitleg: https://www.hersenletsel-uitleg.nl/soorten-hersenletsel-hersenaandoeningen/traumatisch-hersenletsel/subdurale-bloeding-subduraal-hematoom
Hersenstichting - Home. (z.d.). Consulted on 10th may 2016, https://www.hersenstichting.nl/
Homepage van Heliomare. (z.d.). Consulted on 10th may 2016 https://www.heliomare.nl/
Kuks, J. B. M., Snoek, J. W., Oosterhuis, H. G. J. H., & Fock, J. M. (2003). Klinische neurologie (15e ed.). Houten, Nederland: Bohn Stafleu vanLoghum.
Locked in syndroom - Stichting Unlocked. (z.d.). Consulted on 10th januari 2016, van https://www.stichtingunlocked.nl/locked-in/Midline shift
picture with subdural hematoma By James Heilman, MD - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=19364350
Nederlandse Vereniging voor Neurochirurgie - NVvN. (z.d.). Consulted on 10th may 2016, from http://www.nvvn.org/
NVN - Nederlandse Vereniging voor Neurologie :: Home. (z.d.). Consulted on 10th may 2016, from https://www.neurologie.nl/