Epilepsy
Table of Contents
- What is epilepsy
- Epilepsy symptoms and warnings
- Seizures in a brain area or in the entire brain
- Types of seizures
- Epilepsy due to brain injury
- Epilepsy as a cause of brain injury
- What seizures look like
- Treatment (medication or epilepsy surgery)
- First aid for epileptic seizures
- Benefits, disadvantages and risks of epilepsy surgery
What is epilepsy
Epilepsy is an irritation of nerve cells in brain tissue, sometimes accompanied by jerky movements and reduced or absent consciousness.
When we colloquially refer to "the gray matter of our brain," we mean the part of the central nervous system that contains the cell bodies of the nerve cells. The outside of the brain is (brownish) gray, while the inside is (porcelain) white.
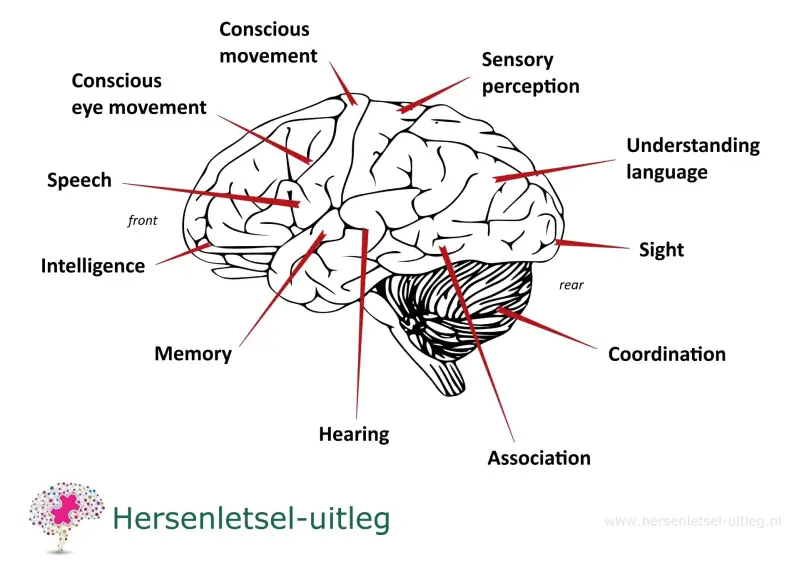
This gray matter consists of several billion gray cells that form networks. These networks each have their own task, focused on a specific function in the body, such as vision, specific movement, hearing, language, smell, and so on.
The image below illustrates this.
The cells in a network communicate with each other through electrical impulses. In epilepsy, a short circuit occurs in one or more networks.
There is a difference in which network with its own specific function a short circuit occurs. That is why epileptic seizures differ from one another.
A seizure can cause a person to be absent for a few seconds to half a minute or even lose consciousness while making jerking movements. But the person may also smell something unusual or fall.
Symptoms that may occur
During an epileptic seizure, a discharge occurs in an area of the brain. The seizure's onset depends on the area of the brain (partial seizure).
Several muscles or muscle groups may contract (motor symptoms). Sensory sensations of smell, taste, touch, or a different perception of time and space may occur. Autonomic reactions such as sweating, blushing, nausea, or palpitations may occur.
If the epileptic disturbance occurs in the area that regulates emotions, people may behave aggressively as a result of an epileptic seizure. Other feelings such as joy, grumpiness, fear, or hallucinations can also occur.
Aura
Some people experience a kind of premonition shortly before a seizure. This can take the form of a strange feeling in the stomach, seeing flashes of light, or hearing strange sounds. This is called an aura.
Prodromes
A person may experience signs days in advance that an attack is "oncoming".
This person may experience abdominal pain, feel unwell, or have a headache. In such cases, this is called a "prodrome."
Seizures localized in the brain or affecting the entire brain
There are two main types of epileptic seizures:
- Partial or focal seizures, affecting one area of the brain
- Generalized epilepsy, affecting both hemispheres of the brain
- Partial (local or focal) seizures: seizures that originate in a specific area of the brain. Consciousness is sometimes intact, sometimes diminished, and sometimes completely absent. Partial epilepsy is the most common form of epilepsy, occurring in over two-thirds of patients. Almost everyone who develops epilepsy after the age of 30 has partial epilepsy. A specific form of partial epilepsy is the Jacksonian march, in which people do not lose consciousness. The seizure occurs on one side of the body. The seizure progresses in a predictable pattern of muscle twitching, tingling, or weakness in a finger, big toe, or the corner of the mouth, after which it marches across the entire hand, foot, or facial muscles for a few seconds.
- Generalized seizures: these seizures involve both hemispheres of the brain. In this case, there is always a disturbance of consciousness, meaning the patient is not or not fully conscious. Approximately 6% of patients have generalized epilepsy.
Types of seizures
- A myoclonic seizure is characterized by muscle twitches in the arms and/or legs, resulting in visible jerks. The person may be conscious and aware of their surroundings, or briefly absent. A myoclonic seizure can be accompanied by atonic seizures (falling or falling). Myoclonic seizures can be caused by genetic conditions or by a lack of oxygen in the brain, for example, after cardiac arrest and successful resuscitation (Lance-Adams syndrome). See other causes of myoclonic seizures on the movement disorders page.
A subcategory is juvenile myoclonic epilepsy (JME), occurring in early puberty or adulthood. The jerks occur primarily in the morning, usually in the shoulders or arms.
- A tonic-clonic seizure is characterized by muscles that both stiffen and jerk. Tonic means cramping, while clonic means jerking. This type of seizure is also called a "major seizure."
- Tonic seizure: In a tonic seizure, the person stiffens and falls to the ground.
- Atonic seizure / drop attack: If the person falls and the muscles become weak, this is called an atonic seizure or a drop attack.
- Clonic seizure: If only rhythmic jerking occurs, this is called a clonic seizure.
- Absence: If a person seems distracted for a moment, stops what he or she was doing, stares, moves the head slightly, or sometimes squirms, this is called an absence.
An absence seizure may last 3-30 seconds.
- A focal seizure with intact awareness is a seizure in one area of the brain (focal). This seizure was previously called a simple partial seizure. Consciousness is intact.
- A focal seizure with impaired consciousness is a seizure in one area of the brain where consciousness is impaired. These seizures were previously called complex partial seizures. The person may be confused.
- Blackouts/brief loss of consciousness are certainly not always an epileptic seizure. It can be syncope, in which the loss of consciousness is caused by reduced blood flow to the brain tissue. This can be the result of a cardiac disorder, but can also be caused by certain neurological disorders of both the central and peripheral nervous systems.
Epilepsy as a cause of brain injury
In some cases, an epileptic seizure can cause brain damage.
This may be caused by a lack of oxygen. Sometimes brain damage occurs after surgery intended to control the seizures.
Epilepsy may result from brain injury
Epilepsy is generally caused by multiple factors. Genetics and environmental factors play a role.
Epilepsy may also result from brain injury. Brain injury occurs when brain cells (neurons) are damaged and die.
Epilepsy resulting from brain injury is most common in people who have had a stroke. In 10% of these people, it occurs with one or more seizures. The risk of epileptic seizures is highest during the first few months after a stroke. Seizures can be either complete or partial.
There is insufficient evidence that administring anti epileptic drugs after a stroke helps prevent the development of epilepsy. Therefore, anti epileptic drugs are not prescribed.
Epilepsy also occurs in:
- traumatic brain injury. The risk of epilepsy increases with the severity of the head trauma, such as skull fractures and penetrating head injuries. The frontal lobe and the temporal lobe are the most commonly affected brain areas.
- brain tumors or metastases of a tumor in the brain
- brain infections, such as meningitis or encephalitis
Tonic-clonic seizure
Myclone seizure
A video about seizures of Medical Centric Podcast
Absence
Impact on daily life
Due to the fact that epilepsy occurs unexpectedly and temporarily takes away autonomy over one's actions, it may have significant consequences for daily life.
People may become insecure or anxious because they never know when a seizure will strike.
Driving with epilepsy is subject to legal regulations.
Stigma
Unfortunately, the stigma attached to this condition is more difficult for many people with epilepsy to cope with than the condition itself.
That is why International Epilepsy Day focuses on this issue.

Treatment
In many cases, medication can prevent epileptic seizures or reduce the risk of seizures. These medications are called antiepileptics. Antiepileptics are effective against certain types of seizures. Not everyone needs antiepileptic medication.
About 75% of people with epilepsy experience seizure freedom with medication. If this is not the case, surgery, for example, can be effective, but it does carry the risk of causing brain damage. For more information about the risks, see the bottom of this page.
For more information about epilepsy treatment, see the websites of some organisations on epilepsy:
https://www.defeatingepilepsy.org/
It is questionable whether administering antiepileptic drugs after a stroke helps prevent the development of epilepsy.
More information on this:
https://eso-stroke.org/prevent-post-stroke-epilepsy-part-2-interventions/
https://www.stroke.org/en/about-stroke/effects-of-stroke/physical-effects/post-stroke-seizures
Surgery
In case epilepsy originates in one hemisphere of the brain or if epilepsy medication doesn't help, epilepsy surgery may be considered.
In same cases a person with epilepsy on both sides of the brain may undergo epilepsy surgery.
Also read about the advantages, disadvantages, and risks of epilepsy surgery.
Resection
In a resection (focal resection), a neurosurgeon removes part of the brain.
Examples of focal resections include:
- temporal lobe lobectomy
- extratemporal lesionectomy, which is the removal of an area outside the temporal lobe
- amygdala-hippocampectomy: removal of the amygdala and hippocampus
- neocortical resection (removal of part of the cerebral cortex)
Resection may be considered for the following conditions:
- cavernous malformation (CCM)
- arteriovenous malformation (AVM)
- tuberous sclerosis
- cortical dysplasia (developmental disorder of the brain and cerebral cortex)
- brain tumors such as DNET, low-grade astrocytoma, or ganglioglioma
Disconnection
A disconnection breaks the connections between parts of the brain.
For example:
- The connection between the left and right hemispheres through the brainbar (corpus callosum): 'callosotomy'.
- The connections between cerebral cortical areas in one hemisphere: 'multiple subpial transection' (MST) using multiple incisions in one hemisphere.
Hemispherectomy
When resection or disconnection is not possible because the epileptic focus is too large or is located in multiple locations, removal of one hemisphere may be considered.
A hemispherectomy can also be performed for Rasmussen's encephalitis (Rasmussen-Kozhevnikov syndrome). This syndrome is characterized by persistent, primarily localized (focal) motor disorders (problems with motor neurons), epilepsy partialis continua, progressive neuropsychological decline with hemiparesis, and cognitive and language deficits.
The encephalitis often begins in the temporal lobe and spreads.
Some websites about hemispherectiomy:
- https://my.clevelandclinic.org/health/procedures/17092-hemispherectomy
- https://www.uclahealth.org/medical-services/pediatric-neurosurgery/conditions-treatment/pediatric-epilepsy-surgery/epilepsy-treatment/hemispherectomy
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4729844/
- https://practicalneurology.com/diseases-diagnoses/epilepsy-seizures/epilepsy-essentials-hemispherectomy-for-early-onset-pediatric-epilepsy-a-big-surgery-for-small-people/32031/
Read about the advantages, disadvantages and risks of epilepsy surgery.
Some websites on epilepsy surgery:
- https://www.epilepsy.com/treatment/surgery
- https://www.mayoclinic.org/tests-procedures/epilepsy-surgery/about/pac-20393981#
- https://www.ncbi.nlm.nih.gov/books/NBK562151/
- https://www.ucsfhealth.org/treatments/focal-resection
- https://academic.oup.com/brain/article/148/6/1866/7978851
- https://www.barrowneuro.org/treatment/epilepsy-surgery/
- https://www.neurosurgeryone.com/treatment/resections/
- https://www.epilepsy.com/treatment/surgery/types
First aid for epileptic seizures
How you should respond depends on the type of seizure.
What NOT to do
- Never put objects or a finger in the mouth. The finger could be bitten off and there is a high risk of choking.
- Do not give anything to drink.
- Do not try to force the mouth open.
- Do not walk away.
What to do BEFORE the seizure (in case the person feels it coming)
- Make the person sit or lie down.
- Reassure the person.
- NEVER give food or drink.
What to do during a seizure
- Try to stay calm.
- Time the seizure. A seizure usually ends within a few minutes.
- Protect the head with your hands or a pillow.
- Make sure the person can't hurt themselves. Remove hard or sharp objects (such as glasses, headphones, necklaces, but also move aside any tables or chairs that could bump into during uncontrolled movements).
- Loosen tight clothing.
- Call an emergency number if the seizure lasts longer than 5 minutes.
- Also call if multiple seizures occur in succession.
- Also call if stroke symptoms occur (crooked mouth, etc.).
- If in doubt, call to discuss the situation.
- Also call if multiple seizures occur in succession.
- Never leave the person alone and reassure him or her once he or she has regained consciousness.
- Do not transport the person.
- Place the person in the recovery position after the tonic and clonic phases.
ADDITION
Sometimes people with epilepsy carry Midazolam nasal spray.
This may be administered a maximum of twice per nostril. It is only necessary in case the person is experiencing a severe tonic-clonic seizure.
What to do after the seizure
- Reassure the person.
- Ask if the person remembers what happened.
- Wait until the person is able to sit or stand.
- Ask family members to support the person.
General tips for people with epilepsy
- Ensure that your medication is taken correctly and at the right times.
- Follow your doctor's advice. For example, don't swim or take a bath without someone present.
- Get enough sleep.
- Avoid stress and tension where possible.
- Tell your loved ones, colleagues, friends, and other acquaintances that you have a form of epilepsy.
- Also tell them which type it is and what they can do in the event of a seizure.
- Warn others if you feel a seizure coming on.
- Carry an ID card with you that explains what people should do in the event of a seizure.
More information:
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/epilepsy-first-aid-and-safety
Pros and cons of epilepsy surgery
Epilepsy surgery is a surgical procedure that removes the part of the brain where the epilepsy originates. This surgery is recommended for people whose focal epilepsy (epilepsy in a specific area) is not helped by medication. Sometimes, problems in a specific part of the brain can also affect other areas.
There is uncertainty about the success of the surgery. In 30% to 40% of patients, seizures continue after surgery. Unfortunately, the medical team cannot accurately estimate this risk.
If the entire epileptic network is not removed, seizures may persist after surgery.
Temporal lobe epilepsy is the most common type of epileptic seizure originating from a single point (focal epilepsy) in the brain.
Research shows that people with TLE (temporal lobe epilepsy) sometimes also have abnormalities in other parts of the brain, not just the hippocampus and temporal lobe (source 1, source 2). These abnormalities together form a network of structures that may be involved in seizures (source 3, source 4, source 5). Epileptic seizures often arise from disruptions in how brain cells connect and work together (source 6, source 7).
Neurosurgeon/epilepsy surgeon P. van Rijen emphasizes the impact of living with epilepsy (source 8).
Of all people with epilepsy, approximately 70% become seizure-free with medication. For the remaining 30%, we can investigate whether surgery is feasible. These people live under enormous pressure. I see people who sometimes have as many as thirty seizures a day. But even one seizure a year can lead to surgery. You never know when it will happen. That feels like a ticking time bomb.” Someone asked if I could operate on her again, for the epilepsy. That was possible, but it meant she would have somewhat less use of her hand afterward. A nearly impossible decision. We talked it over thoroughly, and I operated on her again. She's now seizure-free. The partial loss of her hand function was worth it to her. I understand that completely. It's always a matter of finding the right balance.
Risks and disadvantages of epilepsy surgery
In addition to the advantages mentioned, it is important to mention the risks and disadvantages. Complications may occur.
The Dutch guideline database source 9 for epilepsy surgery states the following:
When considering epilepsy surgery, potential complications should be taken into account. Complications after epilepsy surgery include bleeding and infection (1-2%) (source 10, source 11). This risk is higher with electrode implantations (source 10). After temporal lobe surgery, a (usually non-disabling)
homonymous upper quadrant anopia is common.
Addition by Hersenletsel-uitleg: With this condition, a person can no longer see the upper quadrant (one-quarter) of the visual field on one side. This loss occurs on the same side of both eyes.
Permanent functional loss such as paresis and dysphasia occurs in only 0.6-0.8% of cases (source 10, source 12).
Addition by Hersenletsel-uitleg: People with dysphasia have difficulty pronouncing words, forming sentences, or understanding what others say, even though their intelligence and hearing function normally.
Palsy means partial or incomplete paralysis. It occurs when muscles in the body are weakened, but not completely disabled.
People with palsy may experience mild muscle weakness or a feeling of reduced control over a part of the body, depending on the severity and the cause.
The risk of permanent functional loss (permanent impairment) is higher with surgery outside the temporal lobe (source 10). While epilepsy surgery has little or no long-term positive effect on cognitive functioning (thinking and memory), it does have a positive effect on patients' quality of life (source 13).
This is mainly due to improved social functioning, reduced unemployment, and increased mobility (driving license). (source 14, source 15, source 16)
Patients often have to adjust to the absence of seizures after a life dominated by epilepsy. Some people develop a de novo psychiatric disorder postoperatively, usually depression (source 17).
After surgery, there is usually a reduction in existing psychological complaints, especially depressive ones (source 18).
The disadvantages of hippocampal epilepsy surgery
A common risk of hippocampal epilepsy surgery is memory loss, as the hippocampus plays a key role in processing and storing memories. Other potential side effects include mood swings (changes in a person's emotional state), difficulty learning or concentrating, and, in rare cases, infections or complications from the surgery itself.
The disadvantages of Amygdala Epilepsy Surgery
After amygdala epilepsy surgery patients often report experiencing changes in emotions, such as intense fear or memory problems. The amygdala plays a key role in these functions.
Problems have been reported with the altered emotions and memory, particularly when it comes to recognizing and understanding facial expressions, as well as vision problems and difficulty remembering names and words.
There is no guarantee that the surgical procedure will completely stop epileptic seizures, although the number and severity of seizures are often significantly reduced.
The amygdala and hippocampus, along with other structures, belong to the limbic system.
The limbic system is a complex network of structures in the brain that plays a crucial role in emotions, motivation, memory, and behavior. This system is closely linked to our emotional experiences and influences how we process and store information. It is also not surprising that changes can occur in this area after surgery.
Quote from someone who had both the amygdala and the hippocampus removed:
You go into the surgery with a certain trust in your brain, which has been reacting to situations the same way for 40 years. The healthcare staff has also formed an image of you.
You wake up and suddenly everyone seems angry, aggressive, and you're frightened.
I desperately needed reassurance, explanation, and gentleness. Unfortunately, that wasn't available, and I even underwent EMDR for this fear. I always shared these experiences openly with the hospital, and thankfully, they were very grateful. They said they found it instructive that I could put my experiences into words. But now I live with fear and anxiety over the slightest thing.
Quote from another patient:
I have become an emotional wreck. I'm despondent and sometimes desperate. My emotional regulation is completely destroyed.
The disadvantages of Temporal Lobe Epilepsy Surgery
Temporal lobe epilepsy surgery can be an effective treatment for people who don't respond to medication, but the procedure also carries some potential disadvantages and risks.
First, there is a risk of side effects such as memory problems, since the temporal lobe is involved in
memory and language processing.
Declarative memory, in particular, appears to be affected. (source 20, source 21)
Declarative memory, or explicit memory, is a form of long-term memory in which stored knowledge can be consciously experienced or recalled.
Patients report difficulty remembering new information or retrieving memories.
In addition, there are general risks associated with any surgery, such as infection, bleeding, or complications from anesthesia.
In rare cases, the procedure can lead to changes in mood or personality. It is also possible that the surgery is not completely successful in stopping the epileptic seizures.
It also appears that temporal lobe surgery can cause changes in other parts of the brain, further away from the treated area. Specifically, the thalamus and the fusiform gyrus (where facial recognition takes place) ipsilateral to the side of the surgery. (source 22)
Quote from a mother:
Unfortunately, we weren't properly informed before our son's surgery (three years ago). He's now struggling with many residual symptoms, and thanks to other organizations
(not the hospital), it's only now becoming clear that everything is due to the surgery. But he's seizure-free and medication-free... so the surgery was a success. Fortunately, we're now receiving the right support from others, so hopefully, everyone can learn to cope with it.
Quote from a patient:
I lost my sense of direction and my sense of time, what time it is, etc. That has a major impact.
Quote:
My left temporal lobe was partially removed, as well as the left side of my hippocampus. Your world changes...
Quote:
I have quite a few residual symptoms. Mainly psychological problems. Difficulty expressing my emotions, I get overstimulated very quickly. Depression and sleep problems. It varies greatly for me. That's what makes it so distressing.
The disadvantages of corpus callosum epilepsy surgery
During corpus callosum epilepsy surgery, also called a corpus callosotomy, the connection between the two hemispheres of the brain is partially or completely severed. This can reduce the ability of the brain hemispheres to work together.
This may affect coordination, memory, and information processing.
In addition, patients may experience cognitive changes, such as difficulty multitasking or processing complex tasks.
Other possible side effects include speech problems, reduced motor control, emotional changes.
As with any surgical procedure, there is a risk of complications such as infection, bleeding, or adverse reactions to the anesthesia.
More information
https://my.clevelandclinic.org/health/procedures/17092-hemispherectomy
https://pmc.ncbi.nlm.nih.gov/articles/PMC4729844/
https://www.epilepsy.com/treatment/surgery
https://www.mayoclinic.org/tests-procedures/epilepsy-surgery/about/pac-20393981#
https://www.ncbi.nlm.nih.gov/books/NBK562151/
https://www.ucsfhealth.org/treatments/focal-resection
https://academic.oup.com/brain/article/148/6/1866/7978851
https://www.barrowneuro.org/treatment/epilepsy-surgery/
https://www.neurosurgeryone.com/treatment/resections/
https://www.epilepsy.com/treatment/surgery/types
https://www.epilepsy.com/article/2014/6/understanding-post-traumatic-epilepsy
Information on wikipedia about Dravet syndrome
Patients with this syndrome have epileptic seizures that are usually very difficult to treat and begin in the first year of life.
advertisements are not ours
Resources on epilepsy surgery
Bauman K, Devinsky O, Liu AA. Temporal lobe surgery and memory: Lessons, risks, and opportunities. Epilepsy Behav.2019 Dec;101(Pt A):106596. doi: 10.1016/j.yebeh.2019.106596. Epub 2019 Nov 9. PMID: 31711868; PMCID: PMC6885125
source 21 Cohen NJ, & Squire LR (1980). Preserved learning and retention of pattern-analyzing skill in amnesia: dissociation ofknowing how and knowing that. Science, 210(4466), 207–210. doi: 10.1126/science.7414331 [DOI] [PubMed] [GoogleScholar][Ref list]
source 18 Devinsky, O., Barr, W. B., Vickrey, B. G., Berg, A. T., Bazil, C. W., Pacia, S. V., et al. (2005). Changes in depression andanxiety after resective surgery for epilepsy. Neurology, 65(11), 1744-1749
Freitag, H., & Tuxhorn, I. (2005). Cognitive function in preschool children after epilepsy surgery: rationale for earlyintervention. Epilepsia, 46(4), 561-567
Grivas, A., Schramm, J., Kral, T., von Lehe, M., Helmstaedter, C., Elger, C. E., et al. (2006). Surgical treatment for refractorytemporal lobe epilepsy in the elderly: seizure outcome and neuropsychological sequels compared with a younger cohort.Epilepsia, 47(8), 1364-1372
Hader, W.J., Tellez-Zenteno, J., Metcalfe, A., Hernandez-Ronquillo, L., Wiebe, S., Kwon, C.S., Jette, N. (2013). Complications ofepilepsy surgery: a systematic review of focal surgical resections and invasive EEG monitoring. Epilepsia, 54(5), 840-847
Hemb, M., Palmini, A., Paglioli, E., Paglioli, E.B., Costa da Costa, J., Azambuja, N.,Portuguez, M., Viuniski, V., Booij, L., Nunes,M.L. An 18-year follow-up of seizure outcome after surgery for temporal lobe epilepsy and hippocampal sclerosis. J NeurolNeurosurg Psychiatry. 2013 Jul;84(7):800-5. doi: 10.1136/jnnp-2012-304038. Epub 2013 Feb 13.
source 14 Mohammed, H. S., Kaufman, C. B., Limbrick, D. D., Steger-May, K., Grubb, R. L., Jr., Rothman, S. M., et al. (2012).Impact of epilepsy surgery on seizure control and quality of life: a 26-year follow-up study. Epilepsia, 53(4), 712-720.
Mosewich, R. K., So, E. L., O'Brien, T. J., Cascino, G. D., Sharbrough, F. W., Marsh, W. R., et al. (2000). Factors predictive of theoutcome of frontal lobe epilepsy surgery. Epilepsia, 41(7), 843-849.
source 22 Sainburg LE, Janson AP, Johnson GW, Jiang JW, Rogers BP, Chang C, Englot DJ, Morgan VL. Structural disconnectionrelates to functional changes after temporal lobe epilepsy surgery. Brain. 2023 Sep 1;146(9):3913-3922. doi:10.1093/brain/awad117. PMID: 37018067; PMCID: PMC10473561.
source 11 Sindou, M., Guenot, M., Isnard, J., Ryvlin, P., Fischer, C., & Mauguiere, F. (2006). Temporo-mesial epilepsy surgery:outcome and complications in 100 consecutive adult patients. Acta Neurochir (Wien), 148(1), 39-45.
source 15 Skirrow, C., Cross, J. H., Cormack, F., Harkness, W., Vargha-Khadem, F., & Baldeweg, T. (2011). Long-term intellectualoutcome after temporal lobe surgery in childhood. Neurology, 76(15), 1330-1337.
source 10 Tebo, C. C., Evins, A. I., Christos, P. J., Kwon, J., & Schwartz, T. H. (2014). Evolution of cranial epilepsy surgerycomplication rates: a 32-year systematic review and meta-analysis. J Neurosurg, 120(6), 1415-1427. doi:10.3171/2014.1.jns131694.
source 16 Tellez-Zenteno, J. F., Dhar, R., & Wiebe, S. (2005). Long-term seizure outcomes following epilepsy surgery: asystematic review and meta-analysis. Brain, 128(Pt 5), 1188-1198.
Thomas, S. G., Daniel, R. T., Chacko, A. G., Thomas, M., & Russell, P. S. (2010). Cognitive changes following surgery inintractable hemispheric and sub-hemispheric pediatric epilepsy. Childs Nerv Syst, 26(8), 1067-1073.
Uijl, S. G., Leijten, F. S., Moons, K. G., Veltman, E. P., Ferrier, C. H., & van Donselaar, C. A. (2012). Epilepsy surgery can helpmany more adult patients with intractable seizures. Epilepsy Res, 101(3), 210-216.
source 17 van Veelen, C. W., van Rijen, P. C., Debets, R. M., van Wijk-Leenaars, P. W., & van Emde Boas, W. (2001). [DutchCollaborative Epilepsy Surgery Program: reduction of seizures, operative complications and tapering of medication in 338patients, 1973-1998]. Ned Tijdschr Geneeskd, 145(46), 2223-2228.
Wiebe, S., Blume, W. T., Girvin, J. P., & Eliasziw, M. (2001). A randomized, controlled trial of surgery for temporal-lobe epilepsy.N Engl J Med, 345(5), 311-318.
Zhang K, Hu WH, Zhang C, Meng FG, Chen N, Zhang JG. Predictors of seizure freedom after surgical management of tuberoussclerosis complex: a systematic review and meta-analysis. Epilepsy Res. 2013;105:377-83.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6885125/